Jefferson, in his essay on the nature of concussion (1944), convincingly refuted these vascular hypotheses. Later, Shatsky and coworkers, by the use of high-speed cineangiography, showed displacement of vessels but no arrest of circulation immediately after impact. Beginning with the work of Denny-Brown and Russell in 1941, the physical factors involved in head and brain injury have been subjected to careful analysis. These investigators demonstrated, in the monkey and cat, that concussion resulted when the freely moving head was struck by a heavy mass. If the head was prevented from moving at the moment of impact, the same degree of force invariably failed to produce concussion. More recently, the importance of head motion per se was verified by Gennarelli and colleagues, who were able to induce concussion in primates by rapid acceleration of the head without impact, a condition that rarely occurs in humans. Holbourn, a Cambridge physicist, from a study of gelatin models under conditions simulating head trauma, deduced that when the head is struck, movement of the partly tethered but suspended brain always lags (due to inertia); but inevitably the brain moves also, and when it does it must rotate, for it occupies a round skull whose motions (because of attachment to the neck) usually describe an arc. Pudenz and Sheldon and later Ommaya and coworkers (1974) proved the correctness of this assumption by photographing the brain through a transparent (Lucite) calvarium at the moment of impact. The brain is thus subjected to shearing stresses set up by rotational forces mainly in the sagittal plane centered at its point of tethering in the high midbrain and subthalamus. The torque at the level of the upper reticular formation would explain the immediate loss of consciousness, as described below. Also, these rotational movements of the brain provide a reasonable explanation for the occurrence of surface injuries in certain places, i. These views on the site and mechanism of concussion have been supported by a number of additional physiologic observations. Foltz and Schmidt, in 1956, suggested that the reticular formation of the upper brainstem was the anatomic site of concussive injury. They showed that in the concussed monkey, lemniscal sensory transmission through the brainstem was unaltered, but its effect in activating the high reticular formation was blocked. They also demonstrated that the electrical activity of the medial reticular formation was depressed for a longer time and more severely than that of the cerebral cortex. In 1956 and again in 1961, Strich described the neuropathologic findings in patients who died months after severe closed head injuries that had caused immediate and protracted coma. In all of her cases- in which there were no signs of skull fracture, raised intracranial pressure, or gross subarachnoid hemorrhage- she observed an uneven but diffuse degeneration of the cerebral white matter. In cases of shorter survival (up to 6 weeks), she observed ballooning and interruption of axis cylinders. Adams and colleagues, and by Gennarelli and coworkers, the last of these groups working with monkeys. Strich interpreted the extensive white matter lesions, both in the hemispheres and in the brainstem, to represent a degeneration of nerve fibers that had been stretched or torn by the shear stresses set up during rotational acceleration of the head (diffuse axonal injury), as had been postulated earlier by Holbourn. She suggested that if nerve fibers are stretched rather than torn, the lesions may be reversible and may play a part in the mechanism of concussion. Symonds elaborated this view and saw in the shearing stresses- which are maximal at the point where the cerebral hemispheres rotate on the relatively fixed brainstem. The extension of this idea, namely that diffuse axonal injury throughout the cerebral white matter is the main cause of persistent unconsciousness, has been widely adopted but- as we discuss further on- is open to dispute. Indeed, even the proponents of diffuse axonal injury as an important effect of severe brain damage have found that thalamic lesions are almost always present in cases of prolonged coma or the persistent vegetative state (Adams et al 2000). Clinical Manifestations of Concussion the immediate abolition of consciousness, suppression of reflexes (falling to the ground if standing), transient arrest of respiration, a brief period of bradycardia, and fall in blood pressure following a momentary rise at the time of impact are the characteristic clinical signs of concussive injury. Rarely, if these abnormalities are sufficiently intense, death may occur at the moment of impact, presumably from respiratory arrest. Usually the vital signs return to normal and stabilize within a few seconds while the patient remains unconscious. Brief tonic extension of the limbs, clonic convulsive movements lasting up to about 20 seconds and other peculiar movements may occur immediately after the loss of consciousness (see McCrory et al). These "concussive convulsions" are probably of little significance and have not been shown to confer an increased risk of future seizures.
Clinically, most affected individuals have been mentally retarded and some are epileptic. A degree of hemiparesis may be present, but severe hemispheral neurologic deficits are generally not reported. The hemimegalencephaly has been discovered at autopsy in a few individuals who had no mental or neurologic deficits. Craniostenoses Some of the most startling cranial deformities are caused by premature closure of the cranial sutures (membranous junctions between bones of the skull). Such conditions are estimated to occur in 1 of every 1000 births, with a predominance in males (Lyon and Evrard). The growth of the cranium is inhibited in a direction perpendicular to the involved suture(s), with a compensatory enlargement in other dimensions, as allowed by the patent sutures. For example, when the lambdoid and coronal sutures are both affected, the thrust of the growing brain enlarges the head in a vertical direction (tower skull, or oxycephaly, also referred to as turricephaly and acrocephaly). The orbits are shallow, the eyes bulge, and skull films show islands of bone thinning (Luckenschadel). With premature closure of the coronal suture, the head is excessively wide and short (brachycephalic). If this condition is recognized before 3 months of age, the surgeon can make artificial sutures that may permit the shape of the head to become more normal (Shillito and Matson). Once brain growth has been completed, little can be done aside from complex reconstructive surgery. When several sutures (usually coronal and sagittal) are closed, so as to diminish the cranial capacity, intracranial pressure may increase, impairing cerebral function and causing headache, vomiting, and papilledema. In acrocephalosyndactyly or Apert syndrome, craniostenoses that are combined with syndactyly (fused, or webbed, fingers or toes), there are often added complications- mental retardation, deafness, convulsions, and loss of sight secondary to papilledema. The so-called clover-shaped skull is the most severe and lethal of the craniostenoses because of the associated developmental anomalies of the brain (see further on). When, for any reason, an infant lies with the head turned constantly to one side (because of a shortened sternomastoid muscle or hemianopia, for example), the occiput on that side becomes flattened, as does the opposite frontal bone. The other occipital and frontal bones bulge, so that the maximum length of the skull is not in the sagittal but in the diagonal plane. Craniostenosis of one-half of a coronal suture may also distort the skull in this way. Certain developmental anomalies have been traced to one or another of these stages of cytogenesis and histogenesis in the first trimester of gestation and to the growth and differentiation that take place in the second and third trimesters. During the first trimester of gestation, postmitotic neurons that will ultimately reside in the cortex arise in the ventricular zone adjacent to the ventricles. They then migrate along the scaffold of radial glia to form the multilayered cortex. It is striking that neurons moving up the scaffold must pass through neurons that are already in position in the cortex, leading to an "inside-out" lamination in which the most recently born and arrived neurons reside on the outermost surface of the forming cortex. Originally there is an excess of neurons, many of which degenerate during development- a process properly called apoptosis. There are recorded instances in which the full complement of neuroblasts and neurons fails to be generated. Or the emergence of two separate cerebral hemispheres may not occur (holoprosencephaly), or the bihemispheral brain may remain small (microcephaly). In other described specimens, a diminished number of neurons is less obvious than their failure to migrate to the cortical surface; they remain scattered through the mantle zone in sheets and heterotopic aggregates. It is expressed by a syndrome of mental retardation, seizures, delayed speech, and motor abnormalities. In yet other brains, neuronal migration is normal for the most part, but small groups of neurons in particular regions may lag or present in regional heterotopias (focal dysgeneses). Finally, the cortex may be normally formed and structured but there is a failure of differentiation of intra- and intercor- Disturbances of Neuronal Migration Neuroembryologic studies have identified several milestones of neuroblast formation, migration, cortical organization, neuron dif- Figure 38-1. Deep in the white matter, adjacent to the lateral ventricle, is a large heterotopic aggregate of gray matter. Also, there appears to be an increased infolding of the cerebral cortex (polymicrogyria). The conjunction of cardiac, limb, gut, and bladder abnormalities with neurologic disorder indicates the time at which the insult takes place: cardiac abnormalities occur between the fifth and sixth week; extroversion of the bladder at less than 30 days; duodenal atresia, before 30 days; syndactyly, before 6 weeks; meningomyelocele, before 28 days; anencephaly, before 28 days; cleft lip, before 36 days; syndactyly, cyclopia, and holoprosencephaly, before 23 days.
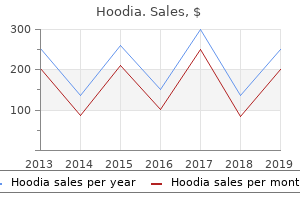
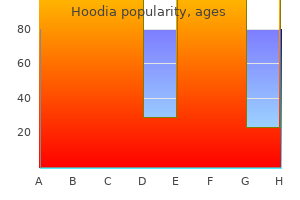
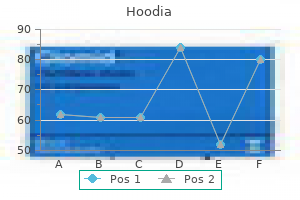
| Comparative prices of Hoodia | ||
| # | Retailer | Average price |
| 1 | Trader Joe's | 431 |
| 2 | ShopKo Stores | 349 |
| 3 | Big Lots | 259 |
| 4 | Family Dollar | 102 |
| 5 | Neiman Marcus | 447 |
Nor is it generally appreciated that the neurologic disorder may have an acute, almost apoplectic onset. In fact, McAlpine and coworkers (1972), who analyzed the mode of onset in 219 patients, found that in about 20 percent the neurologic symptoms were fully developed in a matter of minutes, and, in a similar number, in a matter of hours. In about 30 percent the symptoms evolved more slowly, over a period of a day or several days, and in another 20 percent more slowly still, over several weeks to months. In the remaining 10 percent the symptoms had an insidious onset and slow, steady, or intermittent progression over months and years. The classic relapsing-remitting pattern of disease is more likely to appear in patients who are less than 40 years of age. Early Symptoms and Signs Weakness or numbness, sometimes both, in one or more limbs is the initial symptom in about half the patients. Symptoms of tingling of the extremities and tight bandlike sensations around the trunk or limbs are commonly associated and are probably the result of involvement of the posterior columns of the spinal cord. The symptoms generally appear over a period of hours or days, at times being so trifling that they are ignored, and less often, coming on so acutely and prominently as to bring the partient urgently to the doctor. If the optic neuritis is unilateral, the consensual light reflex from the normal eye is retained. Any pain in the globe is short-lived and persistent pain should prompt an evaluation for local disease. In a cohort of 397 patients enrolled in the Optic Neuritis Treatment Trial and examined 5 years after the initial attack of optic neuritis, visual acuity had returned to 20/25 or better in 87 percent of patients and to 20/40 or better in 94 percent- even if there had been a recurrence of optic neuritis during the 5-year period. Dyschromatopsia, generally taking the form of a perceived desaturation of colors, frequently persists. Once improvement in neurologic function begins, it may continue for several months. The risk is much lower if the initial attack of optic neuritis occurs in childhood [26 percent developed after 40 years of follow-up; Lucchinetti et al (1997)]; this suggests that some instances of the childhood disease may be of a different type, perhaps viral or postinfectious. By far the most common pathologic basis for optic neuritis is demyelinative disease, though it is known that a vascular lesion or compression of an optic nerve by a tumor or mucocele may cause a central or cecocentral scotoma that is indistinguishable from the defect of optic neuritis. Spinal cord lesions have developed months or years later in almost all such cases under our care. The retinal vascular sheathing is due to T-cell infiltration, identical to that in typical plaques, but this is an anomalous finding, since the retina usually contains no myelinated fibers (Lightman et al). The term transverse in relation to the myelitis is somewhat imprecise, implying that all of the elements in the cord are involved in the transverse plane, usually over a short vertical extent. Clinically, the illness is characterized by a rapidly evolving (several hours or days) symmetrical or asymmetrical paraparesis or paraplegia, ascending paresthesias, loss of deep sensibility in the feet, a sensory level on the trunk, sphincteric dysfunction, and bilateral Babinski signs. We have found that fewer than half the patients have evidence of an asymptomatic demyelinative lesion elsewhere in the nervous system or develop clinical evidence of dissemination within 5 years of the initial attack of acute myelitis (Ropper and Poskanzer). Discrete manifestations- such as hemiplegia, trigeminal neuralgia or other pain syndromes, facial paralysis, deafness, or seizures- occur in a small proportion of cases. Most often the disease presents with more than one of the aforementioned symptoms almost simultaneously or in rapid succession. Another relatively isolated syndrome of note, occurring mainly in older women, is a slowly progressive cervical myelopathy with weakness and ataxia. Not infrequently a prominent feature of the disease is nystagmus and ataxia, with or without weakness and spasticity of the limbs- a syndrome that reflects involvement of the cerebellar and corticospinal tracts. Ataxia of cerebellar type can be recognized by scanning speech, rhythmic instability of the head and trunk, intention tremor of the arms and legs, and incoordination of voluntary movements and gait, as described in Chap. But while this group of symptoms is often seen in the advanced stages of the disease, most neurologists would agree that it is not a common mode of presentation. The responsible lesion probably lies in the tegmentum of the midbrain and involves the dentatorubrothalamic tracts and adjacent structures.
Treatment of Infantile and Childhood Hydrocephalus Here one encounters more difficulties than in the treatment of the adult disorder. Peritoneal pseudocysts may form (most shunts in children are ventriculoperitoneal). Another unexpected complication of shunting has been collapse of the ventricles, the so-called slit ventricle syndrome (the appearance of the ventricles on imaging studies is slit-like). This occurs more frequently in young children, though we have observed it in adults. These patients develop a low-pressure syndrome with severe generalized headaches, often with nausea and vomiting, whenever they sit up or stand. To correct the condition, one would imagine that replacing the shunt valve with another that opens under a higher pressure would suffice. But once the condition is established, the most effective measure has been the placement of an antisiphon device, which prevents valve flow when the patient stands. In several large series of cases that have been treated in this way, the number surviving with normal mental function has been small (see review of Leech and Brumback). Mental functions improved unevenly and performance scores lagged behind verbal ones at all levels. Hypercoagulable states (cancer, birth control pills, dehydration, antiphospholipid antibody, etc. Chronic infectious and granulomatous meningitis (fungal, tuberculous, spirochetal, sarcoidosis, etc. As an infrequent idiosyncratic effect of various drugs (amiodarone, quinolone antibiotics, estrogen, phenothiazines, etc. One such form, due to lateral sinus thrombosis, was referred to by Symonds as "otitic hydrocephalus"- a name that he later conceded was inappropriate insofar as the ventricles are not enlarged in this circumstance. This may happen as well with large, high-flow arteriovenous malformations of the brain. The effects of cerebral venous occlusion are considered further in the discussion of pseudotumor cerebri (below) and in Chap. Being a syndrome and not a disease, pseudotumor cerebri has a number of causes or pathogenetic associations (Table 30-1). Actually, the most common form of the syndrome has no firmly established cause- i. Idiopathic Intracranial Hypertension this syndrome was first described in 1897 by Quincke, who called it "serous meningitis. Relatively unremitting but fluctuating headache, described as dull or a feeling of pressure, is the cardinal symptom; it can be mainly occipital, generalized, or somewhat asymmetrical. Other less frequent complaints are blurred vision, a vague dizziness, minimal horizontal diplopia, transient visual obscurations that often coincide with the peak intensity of the headache, or a trifling numbness of the face on one side. Self-audible bruits have been reported by some of our patients; this has been attributed to turbulence created by differences in pressure between the cranial and jugular veins. The risk of visual loss and the severity of headache in many instances make the term benign intracranial hypertension less acceptable. Visual field testing usually shows slight peripheral constriction with enlargement of the blind spots. As vision diminishes, more severe constriction of the fields, with greater nasal or inferior nasal loss, is found. Mentation and alertness are preserved, and the patient seems surprisingly well aside from the headaches, which infrequently becomes severe enough to limit daily activity. As remarked above, most of the patients are overweight young women, often with menstrual irregularities, but the condition also occurs in children or adolescents, in whom there is no clear sex predominance, and in men (Digre and Corbett). Practically all of the women with this disease are obese and so are the men, but to a lesser degree (Durcan et al). All forms of endocrine and menstrual abnormalities (particularly amenorrhea) as well as the use of oral contraceptives have been postulated as causative factors, but none has been substantiated. Karahalios and colleagues and others have found the cerebral venous pressure to be consistently elevated in pseudotumor cerebri; in half of their patients, there was a venous outflow obstruction demonstrated by venography, often with a pressure gradient across the site. In both the aforementioned studies and others like them, the nature of the obstruction was not clear, but the fact that in some series it was bilateral and focal suggests that the stenosis was not simply the passive result of raised intracranial pressure. A related finding in some cases, pointed out to us some time ago by Fishman, is one of partial obstruction of the lateral sinuses by enlarged pacchionian granulations (seen during the venous phase of conventional angiography). For example, 5 of 12 patients treated by Higgins and colleagues became asymptomatic, but this was a population selected by the demonstration of a focal gradient in the lateral sinus during venography.
In this study it was found that the use of intravenous methylprednisolone followed by oral prednisone did indeed speed the recovery from visual loss, although at 6 months there was little difference between patients treated in this way and those treated with placebo. They reported that treatment with oral prednisone alone slightly increased the risk of new episodes of optic neuritis. In a subsequent randomized trial conducted by Sellebjerg and colleagues, it was found that methylprednisolone 500 mg orally for 5 days had a beneficial effect on visual function at 1 and 3 weeks. However, at 8 weeks, no effect could be shown (compared with the placebotreated group), nor was there an effect on the subsequent relapse rate. Glatiramer acetate may be particularly useful in patients who become resistant, i. The rate of such antibody emergence varies directly with the frequency of use of interferon: after a period of years, 30 percent of patients demonstrate antibodies with daily administration, 18 percent with alternate-day use, and less than 5 percent with weekly use. More recent changes in the preparation of interferon have led to reported rates of only 2 percent with antibodies after 1 year of use. There is some evidence that the presence of these antidrug antibodies diminishes the effectiveness of interferon. Antibodies do not develop to glatiramer acetate, and this has been emphasized as a relative advantage of the latter drug. Overall, the side effects of these interferon agents are modest, consisting mainly of flu-like symptoms, sweating, and malaise beginning several hours after the injection and persisting for up to 14 h; they are reduced by nonsteroidal anti-inflammatory drugs and tend to abate with continued use of the agents. There may also be a tendency to depression in susceptible patients treated with interferon, and in our experience, this information, when openly discussed with the patient, has sometimes influenced the decision regarding choice of treatment. A rare but notable problem is the induction of a "systemic capillary leak syndrome" in patients with a monoclonal gammopathy who receive interferon. Patients receiving glatiramer acetate should be warned of an infrequent complication consisting of flushing, chest tightness, dyspnea, palpitations, and severe anxiety. Injection site reactions occur with both classes of drugs but are rarely troublesome if the sites are rotated. From these studies, the concept has emerged that subclinical lesions are of importance and that, over time, cognitive decline and neurologic deficits are more likely to occur if the rate of progression is not reduced by treatment. There are few circumstances where such treatment is mandated immediately and we allow enough time for the patient to consider the alternatives. The endless discussions about the superiority of weekly, every-other-day, or daily medications cannot be resolved except to say that more frequent administration is probably marginally better. In the case of interferon, however, it leads to a higher rate of antibody production over years. With all of these treatments it should be acknowledged that there is no certain correlation between the number of relapses and the ultimate disability despite authoritative statements to the contrary (see Confavreux et al, 2000). The need to treat patients with optic neuritis alone with interferon has not been satisfactorily resolved. We have generally avoided this approach except in a few patients with repeated episodes involving both eyes at various times. Immunosuppressive Drugs A number of agents that modify immune reactivity have been tried, with limited success. Drugs such as azathioprine and cyclophosphamide, as well as total lymphoid irradiation, have been given to small groups of patients and seem to have improved the clinical course of some (Aimard et al, Hauser et al, Cook et al). However, the risks of prolonged use of immunosuppressive drugs, including a chance of neoplastic change, will probably preclude their widespread use. The careful study by the British and Dutch Multiple Sclerosis Azathioprine Trial Group attributed no significant advantage to treatment with this drug. Because this regimen is well tolerated, it may still have some use in otherwise untreatable progressive cases. Among these, mitoxantrone, a drug with broad immunosuppressant and cytotoxic activity used for various cancers, has attracted interest, because one study has shown a slight beneficial effect on the progressive form of the disease (Hartung et al). Mitoxantrone is well tolerated and has the advantage of requiring administration one dose every 3 months (12 mg/m2 intravenously); but it is known from experience with cancer treatment that the total dose is limited by several cardiotoxic effects, including congestive heart failure and arrhythmias.
Syndromes
Cisplatin and carboplatin provide similar marginal improvement in survival beyond that obtained by debulking and radiation therapy. Brachytherapy (implantation of iodine-125 or iridium-193 beads or needles) and high-dose focused radiation (stereotactic radiosurgery) have so far not significantly altered survival times. Almost all glioblastomas recur within 2 cm of their original site and 10 percent develop additional lesions at distant locations. Reoperation is sometimes undertaken for local recurrences, as is brachytherapy, both with uncertain results. The most aggressive approach, a second surgery and chemotherapy, has been generally utilized in patients under age 40 whose original operation was many months earlier. In general, these chemotherapeutic drugs prolong the symptom-free interval but have little effect on survival. With aggressive surgical removal and radiotherapy, as described above, median survival for patients with glioblastoma is 12 months, compared to 7 to 9 months without such treatment. The median survival in cases of anaplastic astrocytoma is considerably longer, 2 to 4 years. Viewed from another perspective, in a recent large series, the 18-month postoperative survival was 15 percent in patients with glioblastoma and 62 percent in those with anaplastic astrocytoma. Favored sites are the cerebrum, cerebellum, hypothalamus, optic nerve and chiasm, and pons. In general, the location of the tumor appears to be influenced by the age of the patient. Astrocytomas of the cerebral hemispheres arise mainly in adults in their third and fourth decades or earlier; astrocytomas in other parts of the nervous system, particularly the posterior fossa and optic nerves, are more frequent in children and adolescents. These tumors are classified further according to their histologic characteristics: protoplasmic or fibrillary; gemistocytic (enlarged cells distended with hyaline and eosinophilic material); pilocytic (elongated, bipolar cells); and mixed astrocytoma-oligodendroglioma types. Some cerebral astrocytomas, as already noted, present as mixed astrocytomas and glioblastomas. These distinctions correlate to a large degree with the biologic behavior of the astrocytomas and therefore have prognostic importance. Cerebral astrocytoma is a slowly growing tumor of infiltrative character with a tendency in some cases to form large cavities or pseudocysts. Other tumors of this category are noncavitating and appear grayish white, firm, and relatively avascular, almost indistinguishable from normal white matter, with which they merge imperceptibly. Fine granules of calcium may be deposited in parts of the tumor, but this finding in a slow-growing intracerebral tumor is more characteristic of an oligodendroglioma. In about half of patients with astrocytoma, the opening symptom is a focal or generalized seizure, and between 60 and 75 percent of patients have recurrent seizures in the course of their illness. Headaches and signs of increased intracranial pressure are relatively late occurrences. Cyst formation and small amounts of calcium are common, especially in cerebellar tumors. The fibrillary tumors have a less stereotyped appearance, generally taking the form of a hypodense mass with less well defined borders and little or no contrast enhancement. The special features of astrocytomas of the pons, hypothalamus, optic nerves, and chiasm, which produce highly characteristic clinical syndromes and do not behave like a cerebral mass, are discussed further on in this chapter. In contrast to glioblastoma, the average survival period after the first symptom is 5 to 6 years in cerebral astrocytomas and 8 years or more in cerebellar ones. Excision of part of a cerebral astrocytoma, particularly the cystic part, may allow survival in a functional state for many years. The cystic astrocytoma of the cerebellum is particularly benign in its overall behavior. In such cases, resection of the tumor nodule is of singular importance in preventing a recurrence. In recent series, the rate of survival 5 years after successful surgery has been over 90 percent (Pencalet et al). The outcome is less assured when the tumor also involves the brainstem and cannot be safely resected. The natural history of the low-grade gliomas is to grow slowly and eventually undergo malignant transformation. The duration of progression and the latency of recurrence with modern treatment may extend for many years. A survey of the outcome of these lowgrade supratentorial tumors showed that 10-year survival after operation was from 11 to 40 percent provided that 5300 cGy was given postoperatively (Shaw et al).
Sometimes in the morning and less frequently when falling asleep, otherwise healthy persons- though awake, conscious, and fully oriented- are seemingly unable to activate their muscles. Respiratory and diaphragmatic function and eye movements are usually not affected, although a few patients have reported a sensation of being unable to breathe. They lie as though still asleep, with eyes closed, and may become quite frightened while engaged in a struggle for movement. They have the impression that if they could move one muscle, the paralysis would be dispelled instantly and they would regain full power. Such attacks are observed in patients with narcolepsy (discussed later in this chapter) and with the hypersomnia of the pickwickian syndrome and other forms of sleep apnea. Usually the attacks are brief (minutes) and transient; if they occur in isolation and only on rare occasions, they are of no special significance. If frequent, as in narcolepsy, they can be prevented by the use of tricyclic antidepressants, particularly clomipramine, which has serotonergic activity. Night Terrors and Nightmares the night terror (pavor nocturnus) is mainly a problem of childhood. The child awakens abruptly in a state of intense fright, screaming or moaning, with marked tachycardia (150 to 170 beats per minute) and deep, rapid respirations. Children with night terrors are often sleepwalkers as well, and both kinds of attack may occur simultaneously. The entire episode lasts only a minute or two, and in the morning the child recalls nothing of it or only a vague unpleasant dream. Children with night terrors and somnambulism do not show an increased incidence of psychologic abnormalities and tend to outgrow these disorders. The persistence of such problems into adult life, however, is said to be associated with significant psychopathology (Kales et al). It has been said that diazepam, which reduces the duration of stages 3 and 4 sleep, will prevent night terrors. Selective serotonin reuptake inhibitors have also been used successfully, especially when night terrors are associated with sleepwalking. Frequent night terrors have reportedly been eliminated by having parents awaken the child for several successive nights, just prior to the usual time of the attack or at the first sign of restlessness and autonomic arousal (Lask). Frightening dreams or nightmares are far more frequent than night terrors and affect children and adults alike. Autonomic changes are slight or absent, and the content of the dreams can usually be recalled in considerable detail. Fevers dispose to them, as do conditions such as indigestion and the reading of bloodcurdling stories or exposure to terrifying movies or television programs before bedtime. Some patients report nightmares when first taking certain medications such as beta blockers, and particularly in our experience, L-dopa. We have also consulted on a few patients who complain of almost nightly nightmares and concurrent severe headaches, but without apparent depression or other psychiatric illness; the nature of their problem is obscure. Persistent nightmares may be a pressing medical complaint and are often accompanied by other behavioral disturbances or neuroses. Somnambulism and Sleep Automatism this condition occurs far more commonly in children (average age, 4 to 6 years) than in adults and is often associated with nocturnal enuresis and night terrors, as indicated above. It is estimated that 15 percent of children have at least one episode of sleepwalking, and that 1 in 5 sleepwalkers has a family history of this disorder. Motor performance and responsiveness during the sleepwalking incident vary considerably. The most common behavioral abnormality is for a patient to sit up in bed or on the edge of the bed without actually walking. When walking about the house, he may turn on a light or perform some other familiar act. There may be no outward show of emotion, or the patient may be frightened (night terror), but the frenzied, aggressive behavior of some adult sleepwalkers, described below, is rare in the child. Usually the eyes are open, and such sleepwalkers are guided by vision, thus avoiding familiar objects; the sight of an unfamiliar object may awaken them.
The brainstem "micturition centers," with their spinal and suprasegmental connections, may contribute. The detrusor muscle receives motor innervation from nerve cells in the intermediolateral columns of gray matter, mainly from the third and also from the second and fourth sacral segments of the spinal cord (the "detrusor center"). These neurons give rise to preganglionic fibers that synapse in parasympathetic ganglia within the bladder wall. Short postganglionic fibers end on muscarinic acetylcholine receptors of the muscle fibers. There are also betaadrenergic receptors in the dome of the bladder, which are activated by sympathetic fibers that arise in the intermediolateral nerve cells of T10, T11, and T12 segments. These preganglionic fibers pass via inferior splanchnic nerves to the inferior mesenteric ganglia. Th 12 Efferent fibers the storage of urine and the efficient emptying of the bladder is possible only when the spinal segments, together L1 Sympathetic with their afferent and efferent nerve fibers, are connected Mesenteric chain L2 plexuses with the so-called micturition centers in the pontomesencephalic tegmentum. In experimental animals, this center (or L3 centers) lies within or adjacent to the locus ceruleus. A medial L4 region triggers micturition, while a lateral area seems more Superior hypogastric important for continence. These centers receive afferent implexus Pelvic nerves pulses from the sacral cord segments; their efferent fibers (presacral n. In cats, the pontomesenganglia 3 cephalic centers receive descending fibers from anteromedial Sacral constriction Plexus o 3 Vas nerves parts of the frontal cortex, thalamus, hypothalamus, and cere4 bellum, but the brainstem centers and their descending path4 ways have not been precisely defined in humans. Other fibers, from the motor cortex, descend with the corticospinal fibers Postganglionic to the anterior horn cells of the sacral cord and innervate the parasympathetic external sphincter. According to Ruch, the descending pathfibers ways from the midbrain tegmentum are inhibitory and those from the pontine tegmentum and posterior hypothalamus are Int. The pathway that descends with the corticospinal nerve tract from the motor cortex is inhibitory. Thus the net effect of lesions in the brain and spinal cord on the micturition reExternal sphincter flex, at least in animals, may be either inhibitory or facilitaFigure 26-5. Almost all of this information has been inferred from animal experiments; there is little human pathologic material to with adrenergically active drugs as well as the more commonly corroborate the role of central nuclei and cortex in bladder control. What information is available is reviewed extensively by Fowler, the external urethral and anal sphincters are composed of striwhose article is recommended. Incleus of Onuf) in the anterolateral horns of sacral segments 2, 3, creased blood flow was detected in the right pontine tegmentum, and 4. When the bladder was full but subjects were prevented from innervate the anal sphincter. The meaning of these lateralized findings is unclear, the pudendal nerves also contain afferent fibers coursing from but the study supports the presumption that pontine centers are the urethra and the external sphincter to the sacral segments of the involved in the act of voiding. These fibers convey impulses for reflex activities and, the act of micturition is both reflex and voluntary. Some of normal person desires to void, there is first a voluntary relaxation these fibers probably course through the hypogastric plexus, as inof the perineum, followed sequentially by an increased tension of dicated by the fact that patients with complete transverse lesions the abdominal wall, a slow contraction of the detrusor, and an asof the cord as high as T12 may report vague sensations of urethral sociated opening of the internal sphincter; finally, there is a relaxdiscomfort. The bladder is sensitive to pain and pressure; these ation of the external sphincter (Denny-Brown and Robertson). It is senses are transmitted to higher centers along the sensory pathways useful to think of the detrusor contraction as a spinal stretch reflex, described in Chaps. Voluntary Unlike skeletal striated muscle, the detrusor, because of its closure of the external sphincter and contraction of the perineal postganglionic system, is capable of some contractions, imperfect muscles cause the detrusor contraction to subside. The abdominal at best, after complete destruction of the sacral segments of the muscles have no power to initiate micturition except when the despinal cord. Isolation of the sacral cord centers (transverse lesions trusor muscle is not functioning normally. The voluntary restraint of the cord above the sacral levels) and their peripheral nerves of micturition is a cerebral affair and is mediated by fibers that permits contractions of the detrusor muscle, but they still do not arise in the frontal lobes (paracentral motor region), descend in the empty the bladder completely; patients with such lesions usually spinal cord just anterior and medial to the corticospinal tracts, and develop dyssynergia of the detrusor and external sphincter muscles terminate on the cells of the anterior horns and intermediolateral (see below), indicating that coordination of these muscles must cell columns of the sacral segments, as described above. With regard to the neurologic diseases that cause bladder dysfunction, multiple sclerosis, usually with urinary urgency, is by far the most common. These data and the physiologic principles elaborated above enable one to understand the effects of the following lesions on bladder function: Complete destruction of the cord below T12, i.
In these severe childhood cases, the deficiencies in cytochrome oxidase suggest a defect in mitochondrial genes, but the site has not been found. As mentioned above, the histologic feature that unites mitochondrial myopathies is the presence of ragged red fibers. This finding points to the diagnosis of a mitochondrial disorder in any case where weakness is coupled with exercise intolerance and elevated serum lactate, particularly if there is a family history of similar problems. Also, the presence of ragged red fibers differentiates the mitochondrial myopathies from the glycogenoses, but it bears emphasizing that ragged red fibers are rare in infants and young children, even in those with confirmed mitochondrial disease. The onset of neurologic difficulty in more than half of these patients is in the first year of life, mostly before the sixth month; but late-onset forms, with great heterogeneity of presentation as late as early adulthood, are also known. Neurologic symptoms often appear subacutely or abruptly, sometimes precipitated by a febrile illness or a surgical operation. It has seemed to us that this rapid onset is more characteristic of Leigh disease than it is of the other mitochondrial disorders. In infants, loss of head control and other recent motor acquisitions, hypotonia, poor sucking, anorexia and vomiting, irritability and continuous crying, generalized seizures, and myoclonic jerks constitute the usual clinical picture. If the onset is in the second year, there is delay in walking, ataxia, dysarthria, psychomotor regression, tonic spasms, characteristic respiratory disturbances (episodic hyperventilation, especially during infections, and periods of apnea, gasping, and quiet sobbing), external ophthalmoplegia, nystagmus, and disorders of gaze (like those of Wernicke disease), paralysis of deglutition, and abnormal movements of the limbs (particularly dystonia but also jerky and choreiform movements). Mild cases, showing mainly developmental delay, have been mistaken for cerebral palsy. Peripheral nerves are involved in some cases (areflexia, weakness, atrophy, and slowed conduction velocities of peripheral nerves); in a few, autonomic failure is the most prominent feature. In some children the disease is episodic; in others it is intermittently progressive and quite protracted, with exacerbation of neurologic symptoms in association with nonspecific infections. The pathologic changes take the form of bilaterally symmetrical foci of spongy necrosis with myelin degeneration, vascular proliferation, and gliosis in the thalami, midbrain, pons, medulla, and spinal cord. The histochemical appearance of muscle is normal, although electron microscopy may show an increased number of mitochondria. A familial disorder of infancy and early childhood- referred to as bilateral striatial necrosis and associated with dystonia, visual failure, and other neurologic defects- is probably a variant. The same may be true of an obscure adult-onset syndrome of progressive dementia, due to thalamic lesions, in the form of necrosis, vascular proliferation, and gliosis. The close relationship between the two processes re-emphasizes the point that several mitochondrial mutations appear to give rise to the clinical and pathologic picture of a subacute necrotizing encephalopathy. Usually there is no diplopia or strabismus or at most only transient diplopia, despite slightly dysconjugate gaze. Mitochondrial abnormalities are found in the extraocular muscles of these patients. We have been impressed at how long the illness can exist before it brings the patient to a physician. To be differentiated is myasthenia gravis, which is characterized by fatigable weakness and responsiveness to cholinergic medications, neither of which is not a feature of mitochondrial disorders. Included in some cases are developmental delay, seizures, and proximal muscle weakness. Santorelli and colleagues found that 12 of 50 patients with Leigh syndrome from 10 families displayed the 8993 point mutation. These differences in severity are thought to result from the mosaicism of mitochondrial genetics and specifically to the protective effect of even small amounts of the normal mitochondrial genome. The first manifestations of disease may not appear until adulthood, although it only rarely begins after age 20. Further confounding the clinical classification of this disease complex is the observation that many patients with the Leigh syndrome have a pyruvate dehydrogenase (usually X-linked) or pyruvate decarboxylase deficiency or a cytochrome oxidase deficiency. These are common to many mitochondrial disorders and inherited usually as an autosomal recessive trait. However, patients with Leigh syndrome and the 8993 mutation tend not to have these enzymatic deficiencies. Bridging these complex cases to the typical ones are instances with cytochrome oxidase deficiency with psychomotor retardation, slowed growth, and lactic acidosis, many without the striatal or brainstem spinal necroses of Leigh syndrome. The process must be distinguished from the several diseases of infancy that are complicated by lactic acidosis.

Sometimes this tumor appears as a complication of an obscure medical condition such as salivary and lacrimal gland enlargement (Mikulicz syndrome). Stereotactic needle biopsy is the preferred method of establishing the histologic diagnosis in sporadic cases. Reduction in the size of the lesion(s) with antimicrobial drugs makes biopsy unnecessary. Treatment Because the tumors are deep and often multicentric, surgical resection is ineffective except in rare instances. Treatment with cranial irradiation and corticosteroids often produces a partial or, rarely, complete response, as remarked above, but the tumor recurs in more than 90 percent of patients. Until recently the median survival of patients treated in this way has been 10 to 18 months, Figure 31-9. Right: Another typical appearance of a smaller ring-enhancing periventricular mass with subtle infiltration of the subependymal regions. In immunocompetent patients, the addition of intrathecal methotrexate and intravenous cytosine arabinoside increases median survival to more than 3 years (DeAngelis), and apparent cure is not unknown. However, this combined treatment is associated with a high risk of a leukoencephalopathy (see further on and. More recent regimens, as outlined by Glass and colleagues, consist of several cycles of intravenous methotrexate (3. The side effects of these treatments are modest and there is no need for repeated lumbar punctures or the placement of an Ommaya reservoir. Most of our patients have not developed mucositis or the other of the usual side effects of this type of chemotherapy. Radiation treatment may be used subsequently, but there is then a higher incidence of delayed leukoencephalopathy and dementia. Corticosteroids are added at any point as needed to control prominent neurologic symptoms. Metastatic Carcinoma Among secondary intracranial tumors, only metastatic carcinoma occurs with high frequency. The pathophysiology of metastatic carcinoma- the complex biologic mechanisms that govern the detachment of tumor cells from the primary growth, their transport to distant tissues, and their implantation on the capillary endothelium of the particular organ in which they will eventually grow- has been well reviewed by Rusciano and Burger and by Posner. Autopsy studies disclose intracranial metastases in approximately 25 percent of patients who die of cancer (Posner). About 80 percent of the metastases are in the cerebral hemispheres and 20 percent in posterior fossa structures, corresponding roughly to the relative size and weights of these portions of the brain and their blood flow. Cancers of the pelvis and colon are exceptional in this respect, having a somewhat higher tendency than this to spread to the posterior fossa. Intracranial metastases assume three main patterns- those to the skull and dura, those to the brain itself, and those spreading diffusely through the craniospinal meninges (meningeal carcinomatosis). Almost as common as intracranial metastases are those to the spinal bones, which in time cause compression of the spinal cord. Metastatic deposits in the spinal cord itself are infrequent but are seen from time to time; they are more common, for example, than a paraneoplastic necrotic myelopathy (see further on). Metastases to the skull and dura can occur with any tumor that metastasizes to bone, but they are particularly common with carcinoma of the breast and prostate and with multiple myeloma. Metastatic tumors of the convexity of the skull are usually asymptomatic, but those at the base may implicate the cranial nerve roots or the pituitary body. Occasionally, a carcinoma metastasizes to the subdural surface and compresses the brain, like a subdural hematoma. Almost one-third of them originate in the lung and half this number in the breast; melanoma is the third most frequent source in most series, and the gastrointestinal tract (particularly the colon and rectum) and kidney are the next most common. Carcinomas of the gallbladder, liver, thyroid, testicle, uterus, ovary, pancreas, etc. Tumors originating in the prostate, esophagus, oropharynx, and skin (except for melanoma) almost never metastasize to the substance of the brain. From a somewhat different point of view, certain neoplasms are particularly prone to metastasize to the brain- 75 percent of melanomas do so, 57 percent of testicular tumors, and 35 percent of bronchial carcinomas, of which 40 percent are small-cell tumors (Posner and Chernik).
References: