Magnetic fields detectable outside the head are produced directly by intracellular current flow in the active neuron. A considerable number of neurons functioning synchronously are necessary to generate electromagnetic fields measurable outside the head. Superficial pyramidal neurons in the gyral crowns contribute to the greatest extent. Magnetic fields due to intracellular currents of radial orientation are cancelled by those of the corresponding extracellular volume currents. The signal of neurons given this orientation will severely be attenuated below the noise level. The sources are localized in cortical sulci or in basal regions of the frontal or temporal lobe, comprising about two thirds of the cortex (see. This follows from the complementary sensitivities of the two techniques (11,20,22,23,2530,53). However, differences in signal-to-noise ratio may also result from different background activities. Most of the typical temporal anterior spikes reflect an activated area of 20 to 30 cm2 (37). Another limiting factor is that the patient has to stay in a shielded room and the acquisition unit is not mobile. The "forward problem" is modeling an electromagnetic field on the surface for a three-dimensionally localized source with defined orientation and strength. There is need for a multilayer and "realistic" head model to simulate a potential field on the surface that takes into account more of the complexities of the individual human head (51). All head models are limited, since conductivity values are rough estimations and age-depending effects are unknown at this time (52). Even the best individual "realistic" head model fails in case of skull breaches or large cystic brain lesions. In the clinical setting, one searches for the localization of the generator, that is, source currents responsible for a given, actually measured extracranial electromagnetic field. Single equivalent current dipole of rhythmic alpha activity (filters 5- and 45-Hz zero-phase). Bottom middle: Results from an invasive recording with subdural grid and depth electrodes confirm preoperative findings (Prof. Chapter 76: Magnetoencephalography 873 Consequently, a priori assumptions of the source structure are necessary in the interpretation of measured data. The equivalent dipole model is the simplest, though nevertheless, mostly applied method. The forward model of an electric dipole is optimized regarding localization, orientation, and strength until it mathematically best fits the measured data. Usually the model with the highest goodnessof-fit (lowest residual variance) serves as the final solution. Usually, only dipole models fulfilling a cutoff criterion for residual variance are regarded as clinically relevant. However, goodness-of-fit may be markedly influenced by background activity, especially in low-amplitude spikes (55). Averaging of similar spikes may improve signal-to-noise ratio and allow for localization of dipoles modeling activity from smaller spikes (55,56). However, single dipoles cannot discriminate activities from multiple, simultaneously active regions. Propagation of epileptic activity may result in such an overlap, and a single dipole will falsely localize the center in between these active regions. Thus, modeling of the spike onset is more important than localization of the peak source (18,32,55,57). Multiple source analysis is another discrete model that considers effects of spatiotemporal propagation and overlapping background activity (18,5860). In contrast to these discrete source models, distributed source models have the advantage that no a priori hypotheses regarding the number of activated regions are needed. However, modeling of hundreds or thousands of electromagnetic sources distributed throughout the solution space is based on the signals of only a limited number of sensors, which results in an underestimation bias.
Syndromes
Liver biopsy shows the characteristic "ductal plate malformation" finding in infants who have congenital hepatic fibrosis. Bacterial infections causing cholestasis can be identified by positive blood or urine cultures. Any history of maternal exposure to , or infection with, toxoplasmosis, syphilis, cytomegalovirus, herpes simplex, varicella zoster, and other viruses should prompt an investigation for such infections. In the case of a suspected viral infection, both serum immunoglobulin M (IgM) and IgG antibodies should be obtained. Hereditary tyrosinemia, a defect of tyrosine metabolism, is suggested by disproportionate abnormalities of hepatic synthetic function, mild abnormalities in bilirubin and ami- Although a myriad of viruses can cause hepatic inflammation, five are primarily hepatotropic: hepatitis A, B, C, D, and E. Although endstage liver disease can occur in up to 10% of patients, fulminant hepatitis rarely has been described. Cases diagnosed in North America have involved patients who imported the virus from abroad. Chronic hepatitis in children is the result of a viral infection; an autoimmune process; exposure to hepatotoxic drugs; or cardiac, metabolic, or systemic disorders. Cholangiography or endoscopic retrograde cholangiopancreatography is necessary to establish the diagnosis. Treatment involves administration of fat-soluble vitamins and ursodeoxy- Copper accumulates in the liver during cholestasis. Other autoimmune diseases may coexist, including thyroiditis, diabetes, hemolytic anemia, and erythema nodosum. Laboratory evaluation reveals elevation of aminotransferases (often very high) and a variable degree of hyperbilirubinemia, the greater part of which is conjugated. Liver biopsy reveals inflammatory infiltrates of the limiting plate and intralobular zones, with piecemeal necrosis, distortion of lobular architecture, and even bridging fibrosis in severe cases. Most acute hepatitis resolves within 3 months in children, after which the etiology of the observed liver disease must be pursued aggressively because many of the diseases causing chronic hepPediatrics in Review Sclerosing cholangitis is characterized by a chronic inflammatory process of the intra- or extrahepatic biliary tree. It may be primary (without evidence of another underlying disease and of unknown etiology) and usually is associated with inflammatory bowel disease. Secondary sclerosing cholangitis results from stones, postoperative strictures, or tumors. Biopsies show a typical concentric fibrosis cholic acid, a naturally occurring choleretic bile acid that appears to improve pruritus in affected patients. Unfortunately, the liver disease progresses in most patients, and cirrhosis develops. Wilson disease is an autosomal recessive disorder caused by a defect in biliary copper excretion, in which excessive copper accumulation leads to cirrhosis. The excess copper is deposited in the cornea, kidneys, and brain, resulting in extrahepatic manifestations of the disease. Although the clinicopathologic presentation may be extremely variable, Wilson disease needs to be included in the differential diagnosis of any child who presents with liver disease, neurologic abnormalities, behavioral changes, or KayserFleischer rings. Serum ceruloplasmin, a carrier of copper, usually, but not invariably, is decreased. Definitive diagnosis requires evaluation of 24-hour urinary copper excretion and copper quantification in liver tissue obtained by biopsy. Wilson disease may present as fulminant hepatic failure, usually in association with a hemolytic crisis due to the toxic effect of copper on red blood cells. Therapy is chelation of copper with penicillamine, which allows for its excretion into the urine. Because the prognosis depends on early treatment and individual responsiveness to chelation therapy, it is important to consider this diagnosis in every child who has signs of chronic liver disease. Ischemic hepatitis results from congestive heart failure, shock (eg, dehydration), asphyxia, cardiorespiratory arrest, or seizures. These novel management strategies are more cost-effective, but also reduce the use of valuable donor livers, making these organs available for patients who do not have other treatment options. In the future, definitive therapy, such as targeted enzyme replacement or gene therapy, may be available for certain metabolic disorders. In view of these exciting prospects, it becomes of great importance to assess the presence of liver disease correctly and quickly in children to allow them to grow and be as healthy as possible until they can reach an age at which definitive therapy may be available. The disorder is due to hypotension/hypoperfusion to the liver during one of the aforementioned events that leads to the liver being damaged as an "innocent bystander" of the original process. Ischemic hepatitis may resemble infectious hepatitis, but it is distinguished easily by rapidly decreasing aminotransferase levels in the days following the initial insult without increasing coagulopathy or hyperbilirubinemia.
This patient may have interictal left occipital discharges that disappear after tumor resection. The Epileptic Lesion the epileptic lesion is a lesion on neuroimaging or pathology that is considered to cause the seizures. Tumors and vascular malformations often have a perilesional epileptogenic zone that is responsible for seizure generation. In other cases, even a partial lesion resection limited by eloquent cortex may render a patient seizure-free. However, history and other investigations may suggest that frequently only one tuber is the epileptic lesion. The Symptomatogenic Zone the symptomatogenic zone is the eloquent area that produces the clinical symptoms when activated during an epileptic seizure. The seizure may start in a clinically silent area and then propagate into eloquent cortical areas. Therefore, the symptomatogenic zone is frequently close to the epileptogenic zone but there may be no direct overlap. The epileptogenic zone is "the area of cortex indispensable for the generation of clinical seizures" (31). The ictal-onset zone is a smaller region within the epileptogenic zone where seizures are generated. The irritative zone is the region that produces interictal epileptiform discharges. This is a lesion on neuroimaging or pathology that is considered to cause the seizures. The symptomatogenic zone is the eloquent area overlapping with the epileptogenic zone that produces the clinical symptoms when activated during an epileptic seizure. The functional deficit zone is the region that functions abnormally during the interictal period. Eloquent cortex is important for generating particular functions, including motor, sensory, language, memory, and other higher cortical functions. In this example, only some motor cortex, somatosensory cortex, visual cortex, and language areas are depicted. The goal of epilepsy surgery is to remove the epileptogenic zone, while at the same time preserving eloquent areas. The Functional Deficit Zone the functional deficit zone is the region that functions abnormally during the interictal period. The functional deficit may be related to interictal epileptiform discharges or to an underlying structural lesion. The functional deficit zone may also be related to functional abnormalities, without structural abnormalities. These authors concluded that interictal epileptiform discharges and seizure spread may influence speech reorganization (46). Binnie showed that frequent interictal spike discharges can lead to impairment during neu- ropsychological testing (44). A "secondary" ictal-onset zone is a different cortical region that is dependent on the primary ictal-onset zone. It is associated with a network of seizure propagation and has potential epileptogenic properties. However, this secondary epileptic focus may disappear after removal of the primary focus. At times, it may also be "independent," and present as a new epileptic focus (47,48). Patients with a prolonged history of seizures before epilepsy surgery have a poorer seizure outcome after resection of the primary focus when compared to individuals with a shorter history of seizures (49). This suggests that secondary epileptogenesis at sites located elsewhere in the brain may develop with persistence of uncontrolled seizures (49). Therefore, it is important to identify the ictalonset zone as well as the associated "epileptic network.
Certain patterns of focal alterations in the biochemical structure may reflect altered neuronal or glial function providing localizing information. Only limited areas of the brain can be studied in a time fashion that is acceptable for clinical practice. It is therefore necessary to have a preimaging hypothesis about the location of epileptogenic focus to decide on the placement of spectroscopy voxels. Multivoxel technique provides the capability of greater anatomic coverage and is particularly appealing if the location of epileptogenic focus is uncertain. Changes in relative quantities of these metabolites, in comparison with corresponding tissue on the presumably normal contralateral hemisphere or controls are used to characterize the tissue metabolically. In patients with bilateral mesial temporal abnormalities, the epilepsy may arise predominantly from one side. In such cases, studies using single-voxel technique comparing the two temporal lobes have provided additional concordant lateralizing information enabling surgical decisions (60,64,65). In a study of nonlesional extratemporal epilepsy, widespread spectroscopic abnormality-greatest in the presumed epileptogenic zone has been reported (67,68). Elevation of "glutamine plus glutamate" in frontal lobes has been reported in idiopathic generalized epilepsies as well (69,70). Anatomic relationships along the lowmiddle convexity: Part I-normal specimens and magnetic resonance imaging. Cortical language localization in left, dominant hemisphere-an electrical stimulation mapping investigation in 117 patients. Relation of cortical language distribution and cognitive function in surgical epilepsy patients. Reorganization of languagespecific cortex in patients with lesions or mesial temporal epilepsy. Mesial temporal sclerosis: diagnosis with fluid-attenuation inversion-recovery versus spin-echo imaging. Non-invasive investigations successfully select patients for temporal lobe surgery. Epilepsy surgery in such cases, when performed often requires invasive intracranial monitoring with subdural grids and depth electrodes, despite which the outcome remains poor. Malformation of cortical development is the most common lesion that evades detection in these cases. Transient splenium lesions in presurgical epilepsy patients: incidence and pathogenesis. Diffusion-weighted magnetic resonance imaging and identification of the epileptogenic tuber in patients with tuberous sclerosis. Susceptibility-weighted imaging for the evaluation of patients with familial cerebral cavernous malformations: a comparison with t2-weighted fast spin-echo and gradientecho sequences. Multimodality imaging of cortical and white matter abnormalities in SturgeWeber syndrome. Enhancing gray-to-white matter contrast in 3T T1 spin-echo brain scans by optimizing flip angle. Curvilinear reconstruction of 3D magnetic resonance imaging in patients with partial epilepsy: a pilot study. Diagnosis of subtle focal dysplastic lesions: curvilinear reformatting from three-dimensional magnetic resonance imaging. Focal cortical dysplasia: improving diagnosis and localization with magnetic resonance imaging multiplanar and curvilinear reconstruction. Microscopic cortical dysplasia in infantile spasms: evolution of white matter abnormalities. The role of 1H magnetic resonance spectroscopy in pre-operative evaluation for epilepsy surgery. Proton magnetic resonance spectroscopic imaging in patients with extratemporal epilepsy.
Prison madness: the mental health crisis behind bars and what we must Do About It. An unanswered health disparity: Tuberculosis among correctional inmates, 1993 through 2003. Full report of the prevalence, incidence, and consequences of violence against women. A national protocol for sexual assault medical forensic examinations: Adults/adolescents. Addressing sexual violence in prisons: A national snapshot of approaches and highlights of innovative strategies. Best correctional practices require administrators to assist victims of prisoner sexual violence. Victims of sexual violence undergo a destructive, catastrophic, life-changing event96 and are, as a result, likely to experience "physical, emotional, cognitive, psychological, social and sexual" problems. The goal for correctional agencies-like sexual assault services in the community-is to assist the individual in making the transition from victim to survivor. Concrete, systematic interventions can help mitigate the life crisis and trauma that results from inmate sexual violence. Many of these issues were identified in the Urban Institute Report, Addressing Sexual Violence in Prisons. When implementing services, correctional officials should consider the importance of choice and active participation by the inmate victim, when this is possible and appropriate. Sexual assault in all forms is the ultimate manifestation of loss of freedom and self-determination, and this is forced upon the victim the individual is powerless to exercise consent over his or her own body and well being. The traumatic event thus destroys the belief that one can be oneself in relation to others. In the community, victims may be unwilling to report out of fear, guilt, shame, and feeling that they will not be believed. If an inmate reports being sexually victimized, he or she may be placed in a very difficult situation:26,27,39,68 staff may respond poorly or blame the victim;43,45 a victim may be placed in protective custody, segregation, or transferred;24 or a victim may be labeled as a "homo" or "punk"106 or "snitch. When inmates believe that their reports will be taken seriously, that they will be provided with adequate protection and safety, when substantive medical and mental health interventions are available and kept confidential, and when discipline and prosecution are used appropriately,40 reporting will be improved. Administrators can invest in multiple, over-lapping, safe and confidential reporting mechanisms that inmates can use. Innovative approaches have been implemented in a number of jurisdictions129 including: Availability and access to no-cost, confidential hotlines to agency investigators, external law enforcement agencies and offices of inspector general; Posters, brochures and other public acknowledgements that identify reporting options and a clear policy that sexual abuse will not be tolerated, reinforced by inmate education and orientation, in clear, understandable language 264 Regular, periodic case reviews with inmates whether by classification, case managers or medical staff, which includes routine questions regarding how safe the inmate feels and whether he/she has ever felt sexually threatened Exit interviews that include questions regarding safety with inmates prior to release, including the use of civilian staff or staff external to the agency Safe mechanisms for victims to file confidential memoranda and/or grievances Ability to confidentially consult with correctional administrators, medical, and mental health staff Access to community rape crisis staff and/or community advocacy staff. Direct supervision environments where officers are stationed in the unit and continually interact with inmates Each contact with an inmate is an opportunity to promote reporting, safety and healing: medical, mental health and classification staff may routinely inquire about inmate safety and victimization to promote reporting and treatment. Since many victims do not report the crime, there are a number of behavioral indicators that might prompt correctional staff to consider whether an inmate has been the victim of prisoner sexual violence. These include: Asking for a room or roommate change Changes in behavior such as acting out to get into segregation Staying in their room Not showering Refusing to participate in an activity that they formerly participated in Substance abuse Suicidal ideation or attempts Self injurious behavior Buying commissary and eating in their room Inmate debt or family transfers to other accounts If staff suspect that an inmate has been victimized, the inmate should be interviewed in an area that avoids raising the suspicions of the inmate population and provides privacy. Correctional agencies, both juvenile and adult, have the obligation to create a safe environment for inmates to report sexual victimization, and to insure that inmates will be kept safe and receive the necessary treatment. Additionally, victims must be placed in housing that will ensure no on-going retribution or continued victimization. Because the inmate now experiences significant loss of freedom, ability to access programs and services, and loss of personal belongings, job and other grounding events,32,39,41,129 the effects of victimization can be increased dramatically. Correctional officials should not automatically default to protective custody for the victim, but should examine the options that exist. When possible, the perpetrator (not victim) should be moved to administrative segregation or outside the institutions. Victims may be placed in cells in closer proximity/scrutiny to correctional staff or in hospital and other more closely supervised units. If it is necessary to move the victim into a more protective environment, care should be taken to avoid disruption of daily life activities, to minimize the deprivations of programs and services available in general population, and to return the victim to a less restrictive environment when appropriate. The goals should be to avoid "labeling" the victim, which can be catastrophic, and to ensure (especially over the long-term) appropriate classification, so that victim and perpetrator will not be re-housed in the same unit or facility in the future. Because correctional environments also have extensive informal networks, consideration of the social consequences especially with other inmates and staff should be considered. The first priority is to treat the imminent physical and life-threatening injuries sustained by the victim, while minimizing disruption to forensic evidence collection. At all times, victims should be treated with dignity, respect and afforded privacy and confidentiality during these difficult interventions.
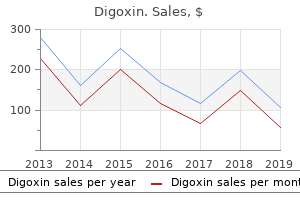
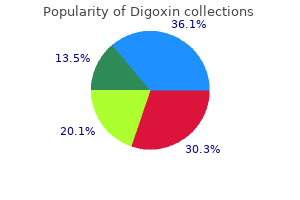
Urginea indica (Squill). Digoxin.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96725
Interestingly, when inmates were asked to identify how frequent they thought sexual assaults were occurring, they had a tendency to overestimate the amount of sexual coercion than was actually recorded. The high sexual coercion rates found in these correctional institutions were specifically correlated with five (5) factors: 1) use of barracks housing, 2) racial conflicts, 3) lax security, 4) prison inmate population over 1,000 and 5) larger inmate population with crimes against persons. The team proffered that "the presence of a sufficient number of motivated security staff and tight security measures appeared to limit sexual coercion among inmates" and also noted that "a facility that used lockdown procedures had a zero rape level" (Struckman-Johnson & Struckman-Johnson, 2000: p. Qualitative Study of Sexual Coercion in One Southern Female Correctional Facility Alarid (2000): Leanne F. The letter writer, Velmarine, was a 41 year old African American mother of three children, serving a 25-year prison term for a third felony conviction who acknowledged being "in the mix" and vividly described both her own experience of sexual coercion and rape and those of other women in this facility. In general, sexual harassment and pressuring occurred more often than sexual assaults, which often went unreported to correctional authorities. Women prisoners who engaged in homosexual relations were most vulnerable to sexual aggression, particularly those women who adopted the masculine role of stud. In general, while rape occurred less often in female prisons, when it did, women were likely to be victimized by multiple perpetrators. Correctional staff need to focus on identifying and curbing sexual coercion, to preempt more aggressive incidents, and need consistent training to understand the dynamics of female sexual coercion, and to hold women accountable for sexual infractions. Alarid (2000) also suggests the use of cameras in vulnerable areas, such as restriction dorms, and inmate orientation to new prisoners, advising them of how to avoid becoming a target, and what assistance is available (legal, medical, psychological) if they are targeted. Inmate Sexual Assault: the Plague Which Persists Dumond, 2000: Dumond (2000) continued his analysis of U. Dumond (2000) noted with alarm that staff sexual misconduct is often ignored in corrections, and he continued to advocate for comprehensive staff training, strong administrative policies and procedures, and sound treatment interventions for victims of sexual assault to meet individual needs and to ensure institutional safety and security. Study of Correctional Officers Attitudes of Homosexuality, Rape, and Prostitution in Male Prisons Eigenberg (2000a): Helen Eigenberg followed up on her previous research in Texas (Eigenberg, 1988) by administering surveys to 391 correctional officers in a mid-western State Department of Correction. Nearly all of the officers (96%) reported "that it was sometimes difficult to tell whether inmates were being forced to participate in sexual acts or if they were willing partners in consensual sexual activities" (Eigenberg, 2000a: p. While most officers in the study collectively indicated they would respond to both consensual sexual acts and rape, they were "consistently less apt to endorse proactive responses to consensual homosexuality than to rape" (Eigenberg, 2000a: p. Similar to her earlier Texas study (Eigenberg, 1988), Eigenberg (2000a) found that a large majority of officers were unwilling to talk to inmates about rape and sexuality in prison as a means of preparing them for this possibility. In an expanded analysis of this data in another journal, Eigenberg (2000b) amplified on these findings, and described the confusion coercion. When an inmate was physically overpowered or threatened with bodily harm, most correctional officers believed an inmate had been raped; however, they were generally less sure about this when coercion was used, and were less willing to define acts of rape when victims were identified as informants. She recommends the use of genderresponsive services and "designing institutional programs and environments that address the unique gender and cultural needs of women" confined in correctional institutions (Greer, 2000: p. National Study on Male Rape by Human Rights Watch No Escape (Mariner, 2001): Joanne Mariner, Esquire of Human Rights Watch conducted the first national study of prisoner sexual violence through research conducted from 1996 through 1999, involving surveys of all 50 state departments of correction and the federal Bureau of Prisons, and information collected from over 200 prisoners in 37 states. The report also provides an extensive review of the case law relevant to prison rape, and vividly documents the serious physical and psychological consequences of prisoner sexual assault for its victims. Of the corrections departments surveyed, only 23 of 46 corrections departments responding maintained distinct statistical information on inmate sexual assault, and only six (6) correctional departments (Arizona, Illinois, Massachusetts, New Hampshire, North Caroline and Virginia and the federal Bureau of Prisons) actually conducted training on prisoner sexual violence (as of 2001). For the most part, criminal prosecution of reported incidents of prisoner sexual violence were virtually non-existent in most jurisdictions. The report outlined a number of deficiencies nationwide: a failure of most correctional agencies in recognizing the reality of prisoner rape and in providing substantive intervention, as well improper classification procedures, negligent doublecelling, understaffing and an in general, an inadequate response to complaints of sexual assault when prisoners come forward. The report provided a number of detailed, substantive recommendations for Federal and State governments to adopt (improved prisoner orientation, adoption of preventative measures, development and initiation of comprehensive intervention strategies for victims, investigation and prosecution of perpetrators, and improved mechanisms to redress legal issues, to name but a few), and set the stage for the national debate to continue. The conference brought together a number of key researchers to examine the problem, and advanced the discussion about the issue, and set the stage for national legislation to be considered. Hensley (2002): In 2002, a contemporary examination on the subject of prison sex was published by Lynne Rienner, under the editorial guidance of Christopher Hensley, and brought together a number of important observations about consensual and nonconsensual sex in prison. Many of the chapters in this text are worthy of note, and have particular applicability in helping correctional administrators manage prison sexual violence. Argot Roles and Prison Sexual Hierarchy (Castle, Hensley, & Tewksbury, 2002): the language of prisoners, known as prison argot, provides insight into the social and cultural milieu of prisons.
At each site, about 4% of patients had a separate, independent assessment done by another emergency department physician within 60 min of the first assessment to check inter-rater reliability. Quality-assurance practices included double and random triple data entry, and annual site monitoring visits. Site investigators, unaware of emergency department data, verified outcomes by medical record review. Follow-up procedures Patients were admitted to the hospital at emergency department physician discretion. To identify missed traumatic brain injuries, research coordinators did standardised telephone surveys of guardians 1162 of patients discharged from the emergency department between 7 and 90 days after the emergency department visit. Medical records and imaging results were obtained if a missed traumatic brain injury was suggested at follow-up. The injury mechanisms were: fall from height (n=11 665, 27%), fall from ground level or ran into stationary object (n=7106, 17%), occupant in motor vehicle crash (n=3717, 9%), head struck by an object (n=3124, 7%), assault (n=2981, 7%), sport-related (n=2934, 7%), fall down the stairs (n=2858, 7%), bicycle collision or fall (n=1668, 4%), pedestrian struck by vehicle (n=1303, 3%), other wheeled transport crash (n=852, 2%), bicyclist struck by automobile (n=524, 1%), other (n=3397, 8%), and unknown (n=283, 1%). Patient characteristics and outcomes were similar between derivation and validation populations (table 1). The corresponding author has access to all data and had final responsibility for the decision to submit for publication. Table 1: Distribution of prediction rule variables and outcomes, according to age group and study phase for more than 24 h for traumatic brain injury and no patients died from the injury. Of the 38 591 discharged, we successfully contacted 30 478 1164 (790%) and reviewed medical records, trauma registries, process improvement reports, and morgue records for the remaining patients. In the derivation and validation groups for children younger than 2 years, 4529 (533%) of 8502, and 1176 (531%) of 2216 patients, respectively, had none of the six predictors in the rule (figure 2A): altered mental status, non-frontal scalp haematoma, loss of consciousness for 5 s or more, severe injury mechanism, palpable skull fracture, or not acting normally according to the parent. In the derivation and validation groups for children aged 2 years and older, 14 663 (580%) of 25 283, and 3800 (593%) of 6411, respectively, had none of the six predictors in the rule (figure 2B): abnormal mental status, any loss of consciousness, history of vomiting, severe injury mechanism, clinical signs of basilar skull fracture, or severe headache. Although the predictor vomiting was assessed in several different forms (presence, number, and timing), its simple presence was identified as the most useful form in the prediction tree. In the validation group, the prediction rule had a negative predictive value of 3798/3800 (9995%, 99819999), and sensitivity of 61/63 (968%, 890996). One was a non-helmeted bicyclist who sustained multisystem trauma including substantial pulmonary injuries. The second patient was a non-helmeted inline skater who skated down more than ten steps, and had a moderate headache and a large frontal scalp haematoma. Point estimates for the test characteristics of the prediction rules in both age groups were similar between derivation and validation populations. Other signs of altered mental status: agitation, somnolence, repetitive questioning, or slow response to verbal communication. Severe mechanism of injury: motor vehicle crash with patient ejection, death of another passenger, or rollover; pedestrian or bicyclist without helmet struck by a motorised vehicle; falls of more than 09 m (3 feet) (or more than 15 m [5 feet] for panel B); or head struck by a high-impact object. Additionally, the lack of validation studies compromises the generalisability of previous rules. The current study is very large, allowing sufficient statistical power to generate robust and generalisable rules. Similarly, our study also excluded asymptomatic children with very-low-risk injury mechanisms, to avoid overinflating the negative predictive value. The extent of this reduction is unclear, however, as not all children outside We obtained follow-up, however, which is an acceptable alternative when definitive testing is not feasible or ethical. Assignment of a higher relative cost could improve rule sensitivity (at the risk of losing specificity). When we re-analysed the data with a cost ratio of 1000 to 1, however, the variable sequence in the tree did not change. Sensitivities of the derived prediction rules were high but not perfect, which is difficult to achieve in a study of this size. The high rule sensitivities, however, were almost identical in both the derivation and validation populations, increasing the validity of the rule. As with other decision-support tools, however, these rules are meant to inform clinician, not to replace their decision making. A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated?
Both exogenous (other highly protein-bound medications) and endogenous (increased bilirubin) substances can compete for binding sites and increase unbound phenytoin concentrations. Valproic acid significantly alters phenytoin binding to serum albumin, whereas phenobarbital, ethosuximide, diazepam, carbamazepine, and folic acid do not (36). In patients with uremia who undergo renal transplantation, binding returns to normal when renal function recovers (38). Total phenytoin concentrations that are below the normal range can be associated with unbound phenytoin concentrations in the therapeutic range. For example, if a patient has a subtherapeutic total phenytoin concentration of 5 g/mL but an unbound fraction of 20%, the equivalent unbound phenytoin concentration is 1 g/mL, which is in the "therapeutic" range. Thus patients at high risk for altered protein binding may respond to clinically subtherapeutic total concentrations and may not tolerate total serum concentrations within the therapeutic range. If such patients experience toxic reactions despite therapeutic concentrations, measurement of unbound concentrations may be warranted. Total phenytoin concentrations may be a misleading test in developing countries, where hypoalbuminemia is highly prevalent (39). Among the methods that predict total phenytoin concentrations in the face of reduced albumin levels, the best documented is the Sheiner-Tozer method (40,41): Cn Co/(0. An arene oxide, which precedes the formation of these compounds, has been implicated in the toxicity and teratogenicity of phenytoin; however, its transient presence in patients with normally functioning arene oxide detoxification systems is unlikely to account for many of the toxic reactions (49,50). Individuals homozygous for the wild-type allele are called extensive metabolizers. Individuals with at least one of these variant alleles are called poor metabolizers and have a reduced ability to metabolize phenytoin. They may require lower-than-average phenytoin doses to decrease the incidence of concentration-dependent adverse effects (57,63). These two variant alleles are much less prevalent in African Americans and Asians, with more than 95% of these groups expressing the wild-type genotype (51). A clear association between the newer discovered alleles and an altered phenytoin metabolism has not yet been demonstrated. Moreover, the mean phenytoin maintenance dose leading to a therapeutic serum where C o is the measured total phenytoin concentration (milligrams/liter), Alb is albumin concentration (grams/ deciliter), and Cn is the total phenytoin concentration that would have been observed with normal albumin concentrations. Phenytoin is distributed freely in the body with an average volume of distribution in humans of 0. At the pH of plasma, phenytoin exists predominantly in the nonionized form, thus allowing rapid movement across cell membranes by nonionic diffusion. The volume of distribution, which correlates with body weight (43), is larger in morbidly obese patients, who may require large loading doses to achieve therapeutic concentrations (44,45). The patient showed signs of central nervous system intoxication, ataxia, and diplopia (58). In another Japanese study (54), the predicted plasma concentrations with a phenytoin dose of 5 mg/kg/day were 18. Relationship between serum phenytoin concentration and daily dose in five patients. Enzyme saturation kinetics lead to phenytoin plasma concentrations increasing nonproportionally with changes in dose. The relationship between dose and concentration can be expressed by the MichaelisMenten equation: Dose (mg/day) VmaxCss Km Css where Vmax is the maximal rate of drug metabolism, Css the steady-state serum concentration, and Km the concentration at which Vmax is half-maximal. In most patients, phenytoin exhibits nonlinear pharmacokinetics because the usual therapeutic plasma concentrations exceed the usual Km. Concomitant illnesses (86) or medications, pregnancy (87,88), genetic makeup (8991), and age can significantly affect Vmax or Km (or both). Children have higher Vmax values, but similar Km values, compared with adults (9294); elderly individuals have lower Vmax values (mean, 6. Excretion Up to 95% of phenytoin is excreted in urine and feces as metabolites, with 5% or less of unchanged phenytoin excreted in urine. Some investigators have suggested that phenytoin enhances its own elimination through enzyme induction (96).
Provide on-going care as the primary physician to their continuity clinic patients, and be available to their patients at all times during office hours and arrange coverage for their patients when they are unavailable 13. Satisfactory performance of the above responsibilities as assessed by faculty evaluations and 360 degree evaluations during the clinical rotations 2. Show evidence of ability to manage increasingly complex medical problems using appropriate consultants 3. Work efficiently and cooperate with the health care team, avoid iatrogenic problems, anticipate and prevent impending problems, and recognize additional co-existing problems 4. Meet licensing requirements as deemed necessary by the Kansas State Board of Healing Arts 10. Demonstrate the ability to function as an independent clinician with the ability to manage simple to complex problems and conditions and direct/assess day-to-day patient care 6. Teach junior residents and students how to diagnosis and manage commonly seen general and subspecialty problems 10. Provide on-going care as the primary physician to their continuity clinic patients, and be available to their patients at all times during office hours and arrange coverage for their patients when they are unavailable 11. Communicate regularly with the patient, the family, and the referring physician 13. Other expectations as outlined in "Performance Expectations" 20 Criteria for Graduation from the Program 1. Recertification of Basic Life Support, Neonatal Resuscitation Program and Pediatric Advance Life Support training 3. Additional reviews may be needed for residents experiencing academic or professional difficulties. The previous degree must match the official degree earned and shall not be converted to equivalent degrees. For foreign medical institutions, the official degree conferred is verified by searching the Foundation for Advancement of International Medical Education and Research database. This database is endorsed by the Educational Commission for Foreign Medical Graduates. Additional information on the Evaluations can be found in the University of Kansas Graduate Medical Education Policy and Procedure Manual. Non-compliance or inability to meet the required outcomes may lead to these reportable interventions by the Program. When a resident has a negative interaction with a patient, is that Interpersonal and Communication Skills or Professionalism? When a resident is not ready to present their conference on time is that PracticeBased Learning and Improvement or Professionalism? Part of your growth in training will be to develop the professionalism expected of pediatricians. Professionalism is defined by demonstrating commitment to carrying out professional responsibilities and in adherence with ethical principles. Residents are expected to demonstrate compassion, integrity, excellence, altruism, and respect for others; responsiveness to patient needs; respect for patient privacy; accountability to patients, society and the profession; honesty and dependability; and sensitivity and responsiveness to a diverse patient population including but not limited to gender, age, culture, race, religion, disabilities and sexual orientation. We know that residency is stressful and the hours can be long and this kind of environment is guaranteed to produce lapses in professionalism. Sometimes this involves meeting with an attending, your advisor, the Pediatric Chief or a Program Director. We also use Professionalism calls as detailed in the Pediatric Residency Policies and Procedures Manual. These calls are assigned to residents who have inconvenienced a colleague or patients because of a lack of professionalism. For example, if you forget to double check the clinic schedule and miss a continuity clinic that then must be covered by your peers, you will get a professionalism call. The University of Kansas School of Medicine projects an image of professionalism within our community. Faculty Advisor/Mentors Each resident will be assigned a faculty advisor or mentor, usually a General Pediatrician or BehavioralDevelopmental Pediatrician, for their junior year. If over the course of residency the resident chooses to switch advisors or add a specialty advisor, such changes are permitted with the approval of the Program Director.
Determine if patient is under the care of mental health professionals and record contact information. If patient refuses care, contact police if unable to convince patient to be transported. For patient with suspected Excited/Agitated Delirium: Treat hyperthermia, see Hyperthermia Protocol 2. F Facilitate identification and activation of resources (clergy, family, friends, or police). R Recovery/referral - leave patient in the care of a responsible person, professional or transport to appropriate medical facility. Expose as necessary to assess for bleeding/discharge, crowning, prolapsed cord, breech, limb presentation Do not digitally examine or insert anything into the vagina. For patients with suspicion of hyperthermia/heatstroke, treat per Hyperthermia Protocol 2. The following symptoms, when associated with a fever, suggest a more serious illness: Persistent vomiting Severe headache Difficulty breathing Unusual sensitivity to bright light Chest pain Severe swelling of the throat Extreme listlessness or irritability Stiff neck and pain when the head is bent forward Abdominal pain Unusual skin rash Pain when urinating Confusion For patients where transport is refused, urge caregivers to observe for signs of serious illness, encourage appropriate fluid intake, and safely store antipyretics. The primary goal of treating fever is increased comfort rather than normalization of body temperature. There is no evidence that fever worsens illness or causes long-term neurologic complications. Note: Reassess patient between each bolus for improving clinical signs and signs of volume overload (rales, increased work of breathing, or increased oxygen requirements). Signs and symptoms of Diabetic Ketoacidosis include uncontrolled blood glucose greater than or equal to 250 mg/dL, weakness, altered mental status, abdominal pain, nausea, and vomiting, polyuria (excessive urination), polydipsia (excessive thirst), a fruity odor on the breath (from ketones), and tachypnea. Common causes of Diabetic Ketoacidosis include infection, acute coronary syndrome, and medication non-compliance. Most patients present with severe dehydration and focal or global neurological deficits. Hyperglycemia may be detrimental to patients at risk for cerebral ischemia such as victims of stroke, cardiac arrest, and head trauma. For serum lab value 6 mmol/L, request paramedic if available but do not delay transport. Some clinical factors predisposing patients to hyperkalemia: o Chronic renal failure o Acute renal failure (may be secondary to dehydration, shock, nephrotoxins, obstruction, etc. The electrophysiological effects of hyperkalemia are proportional to both the potassium level and its rate of increase. If temperature is >1040F (400C) or if altered mental status is present, begin active cooling by: o Continually misting the exposed skin with tepid water while fanning the victim (most effective). Immersion cooling is the most effective method to lower core body temperature if proper resources are available. Hyperthermia: Elevated temperature may be due to environmental exposure, pharmacologic agents, or excited (agitated) delirium, see Behavioral Emergencies Protocol 2. Mortality and morbidity are directly related to the length of time the victim is subject to the heat stress. D10% may benefit patients by decreasing the likelihood of post-treatment hyperglycemia and reducing the likelihood of extravasation injury. Causes of hypoglycemia include medication misuse or overdose, missed meal, infection, cardiovascular insults. Patients with corrected hypoglycemia who are taking these agents are at particular risk for recurrent symptoms and frequently require hospital admission. Providers are encouraged to administer additional dosages while transporting to the Emergency Department. Hypoglycemia may be detrimental to patients at risk for cerebral ischemia, such as victims of stroke, cardiac arrest, and head trauma. A minimum of 45 60 second assessment of respirations and pulse is necessary to confirm respiratory arrest or cardiac arrest. Impaired consciousness, not shivering <32 to 28°C Cardiac monitoring, minimal and cautious movements to avoid arrhythmias, horizontal position and immobilization, full-body insulation, active external and minimally invasive re-warming techniques (warm environment; chemical, electrical, or forced-air heating packs or blankets; warm parenteral fluids). Hypothermic patients are often significantly dehydrated, and may require repeat fluid boluses.
References: