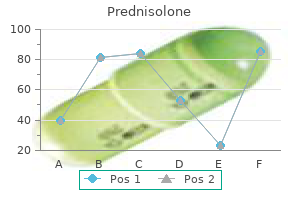
In other words, the contrasting parental traits were expected to blend in the offspring. He allowed the F1 plants to self-fertilize and found that, of F2generation plants, 705 had violet flowers and 224 had white flowers. When Mendel transferred pollen from a plant with violet flowers to the stigma of a plant with white flowers and vice versa, he obtained about the same ratio regardless of which parent, male or female, contributed which trait. This is called a reciprocal cross-a paired cross in which the respective traits of the male and female in one cross become the respective traits of the female and male in the other cross. For the other six characteristics Mendel examined, the F1 and F2 generations behaved in the same way as they had for flower color. One of the two traits would disappear completely from the F1 generation only to reappear in the F2 generation at a ratio of approximately 3:1 (Table 12. Recessive traits become latent, or disappear, in the offspring of a hybridization. The recessive trait does, however, reappear in the progeny of the hybrid offspring. For this same characteristic (flower color), white-colored flowers are a recessive trait. The fact that the recessive trait reappeared in the F2 generation meant that the traits remained separate (not blended) in the plants of the F1 generation. Mendel also proposed that plants possessed two copies of the trait for the flower-color characteristic, and that each parent transmitted one of its two copies to its offspring, where they came together. Moreover, the physical observation of a dominant trait could mean that the genetic composition of the organism included two dominant versions of the characteristic or that it included one dominant and one recessive version. Conversely, the observation of a recessive trait meant that the organism lacked any dominant versions of this characteristic. To understand how Mendel deduced the basic mechanisms of inheritance that lead to such ratios, we must first review the laws of probability. The empirical probability of an event is calculated by dividing the number of times the event occurs by the total number of opportunities for the event to occur. It is also possible to calculate theoretical probabilities by dividing the number of times that an event is expected to occur by the number of times that it could occur. Theoretical probabilities come from knowing how the events are produced and assuming that the probabilities of individual outcomes are equal. A probability of one for some event indicates that it is guaranteed to occur, whereas a probability of zero indicates that it is guaranteed not to occur. In his experiment, Mendel demonstrated that the probability of the event "round seed" occurring was one in the F1 offspring of true-breeding parents, one of which has round seeds and one of which has wrinkled seeds. When the F1 plants were subsequently self-crossed, the probability of any given F2 offspring having round seeds was now three out of four. In other words, in a large population of F2 offspring chosen at random, 75 percent were expected to have round seeds, whereas 25 percent were expected to have wrinkled seeds. Using large numbers of crosses, Mendel was able to calculate probabilities and use these to predict the outcomes of other crosses. The Product Rule and Sum Rule Mendel demonstrated that the pea-plant characteristics he studied were transmitted as discrete units from parent to offspring. As will be discussed, Mendel also determined that different characteristics, like seed color and seed texture, were transmitted independently of one another and could be considered in separate probability analyses. For instance, performing a cross between a plant with green, wrinkled seeds and a plant with yellow, round seeds still produced offspring that had a 3:1 ratio of green:yellow seeds (ignoring seed texture) and a 3:1 ratio of round:wrinkled seeds (ignoring seed color). The product rule of probability can be applied to this phenomenon of the independent transmission of characteristics. The product rule states that the probability of two independent events occurring together can be calculated by multiplying the individual probabilities of each event occurring alone. To demonstrate the product rule, imagine that you are rolling a sixsided die (D) and flipping a penny (P) at the same time. The outcome of rolling the die has no effect on the outcome of flipping the penny and vice versa. Twelve Equally Likely Outcomes of Rolling a Die and Flipping a Penny Rolling Die D1 D1 D2 D2 D3 D3 D4 D4 D5 D5 D6 D6 Table 12. The sum rule states that the probability of the occurrence of one event or the other event, of two mutually exclusive events, is the sum of their individual probabilities.

The usual organisms (and with time there is always a mixed infection) are Staphylococcus aureus, Escherichia coli, Streptococcus pyogenes, Proteus mirabilis and Pseudomonas aeruginosa; in the presence of foreign implants Staphylococcus epidermidis, which is normally non-pathogenic, is the commonest of all. The host defences are inevitably compromised by the presence of scar formation, dead and dying bone around the focus of infection, poor penetration of new blood vessels and non-collapsing cavities in which microbes can thrive. There is also evidence that bacteria can survive inside osteoblasts and osteocytes and be released when the cells die (Ellington et al. The commonest of all predisposing factors is local trauma, such as an open fracture or a prolonged bone operation, especially if this involves the use of a foreign implant. Treatment the essence of treatment is prophylaxis: thorough cleansing and debridement of open fractures, the provision of drainage by leaving the wound open, immobilization of the fracture and antibiotics. In most cases a combination of flucloxacillin and benzylpenicillin (or sodium fusidate), given 6-hourly for 48 hours, will suffice. If the wound is clearly contaminated, it is wise also to give metronidazole for 4 or 5 days to control both aerobic and anaerobic organisms. The presence of necrotic soft tissue and dead bone, together with a mixed bacterial flora, conspire against effective antibiotic control. Treatment calls for regular wound dressing and repeated excision of all dead and infected tissue. Traditionally it was recommended that stable implants (fixation plates and medullary nails) should be left in place until the fracture had united, and this advice is still respected in recognition of the adage that even worse than an infected fracture is an infected unstable fracture. However, advances in external fixation techniques have meant that almost all fractures can, if necessary, be securely fixed by that method, with the added advantage that the wound remains accessible for dressings and superficial debridement. If these measures fail, the management is essentially that of chronic osteomyelitis. Pathology Bone is destroyed or devitalized, either in a discrete area around the focus of infection or more diffusely along the surface of a foreign implant. In the worst cases a sizeable length of the diaphysis may be devitalized and encased in a thick involucrum. Sequestra act as substrates for bacterial adhesion in much the same way as foreign implants, ensuring the persistence of infection until they are removed or discharged through perforations in the involucrum and sinuses that drain to the skin. The young boy (a) presented with draining sinuses at the site of a previous acute infection. Bone destruction, and the increasingly brittle sclerosis, sometimes results in a pathological fracture. The histological picture is one of chronic inflammatory cell infiltration around areas of acellular bone or microscopic sequestra. In longstanding cases the tissues are thickened and often puckered or folded inwards where a scar or sinus adheres to the underlying bone. Organisms cultured from discharging sinuses should be tested repeatedly for antibiotic sensitivity; with time, they often change their characteristics and become resistant to treatment. Note, however, that a superficial swab sample may not reflect the really persistent infection in the deeper tissues; sampling from deeper tissues is important. The most effective antibiotic treatment can be applied only if the pathogenic organism is identified and tested for sensitivity. Unfortunately standard bacterial cultures still give negative results in about 20% of cases of overt infection. However, although this has been shown to reveal unusual and otherwise undetected organisms in a significant percentage of cases, the technique is not widely available for routine testing. A range of other investigations may also be needed to confirm or exclude suspected systemic disorders (such as diabetes) that could influence the outcome. However, there are marked variations: there may be no more than localized loss of trabeculation, or an area of osteoporosis, or periosteal thickening; sequestra show up as unnaturally dense fragments, in contrast to the surrounding osteopaenic bone; sometimes the bone is crudely thickened and misshapen, resembling a tumour. The least serious, and most likely to benefit, are patients classified as Stage 1 or 2, Type A, i. Type C patients are so severely compromised that the prognosis is considered to be poor.
Placing the pins is made easier if two temporary pins are first inserted hugging the medial and lateral surfaces of each iliac blade and then directing the fixing pins between them. Internal fixation by attaching a plate across the symphysis should be performed: (1) during the first few days after injury only if the patient needs a laparotomy; and (2) later on if the gap cannot be closed by less radical methods. However, if displacement is marked, or if there is an associated anterior ring fracture or symphysis separation, then open reduction and internal fixation with plates and screws will need to be considered. It is also possible to reduce and hold some of these fractures by external fixation. It may be possible to reduce some or all of the vertical displacement by skeletal traction combined with an external fixator; even so, the patient needs to remain in bed for at least 10 weeks. As these injuries represent loss of both anterior and posterior support, both areas will need to be stabilized. Two techniques are used: (a) anterior external fixation and posterior stabilization using screws across the sacroiliac joint, or (b) plating anteriorly and iliosacral screw fixation posteriorly. Posterior operations are hazardous (the dangers include massive haemorrhage, neurological damage and infection) (a) (b) (c) 836 28. Persisting with skeletal traction and external fixation is probably safer, though the malposition is likely to leave a legacy of posterior pain. It should be emphasized that more than 60 per cent of pelvic fractures need no fixation. Acetabular fractures combine the complexities of pelvic fractures (notably the frequency of associated soft-tissue injury) with those of joint disruption (namely, articular cartilage damage, noncongruent loading and secondary osteoarthritis). The fractures are divided into four major types; though they are distinguished on anatomical grounds, it is important to recognize that they also differ in their ease of reduction, their stability after reduction and their long-term prognosis. Acetabular wall fractures Fractures of the anterior or posterior part of the acetabular rim affect the depth of the socket and may lead to hip instability unless they are properly reduced and fixed. Complications Thromboembolism A careful watch should be kept for signs of deep vein thrombosis or pulmonary embolism (Montgomery et al. Sciatic nerve injury It is essential to test for sciatic nerve function both before and after treating the pelvic fracture. If the nerve is injured it is usually a neuropraxia and one can afford to wait several weeks for signs of recovery. Urogenital problems Urethral injuries sometimes result in stricture, incontinence or impotence and may require further treatment. Persistent sacroiliac pain Unstable pelvic fractures are often associated with partial or complete sacroiliac joint disruption, and this can lead to persistent pain at the back of the pelvis. On the x-ray it is shown in profile by the iliopectineal line in the oblique view. Anterior column fractures are uncommon, do not involve the weightbearing area and have a good prognosis. The posterior column extends from the ischium, across the posterior aspect of the acetabular socket to the sciatic notch and the posterior part of the innominate bone. A posterior column fracture usually runs upwards from the obturator foramen into the sciatic notch, separating the posterior ischiopubic column of bone and breaking the weightbearing part of the acetabulum. It is usually associated with a posterior dislocation of the hip and may injure the sciatic nerve. Treatment is more urgent and usually involves internal fixation to obtain a stable joint. A vertical split into the obturator foramen may coexist, resulting in a T-fracture. Note that in both transverse and T-type fractures, a portion of the acetabulum remains attached to the ilium. The obturator oblique (a), standard anteroposterior (b) and iliac oblique (c) views will allow the trained eye to picture the structures involved in the injury. The iliopectineal line represents a profile of the anterior column whereas the ilioschial line defines the posterior column.
As with femoral neck fractures, they are common in elderly, osteoporotic people; most of the patients are women in the 8th decade. However, in contrast to intracapsular fractures, extracapsular trochanteric fractures unite quite easily and seldom cause avascular necrosis. The leg is shorter and more externally rotated than with a transcervical fracture (because the fracture is extracapsular) and the patient cannot lift his or her leg. Mechanism of injury the fracture is caused either by a fall directly onto the greater trochanter or by an indirect twisting injury. The crack runs up between the lesser and greater trochanter and the proximal fragment tends to displace in varus. The lesser and greater trochanters may be identifiable as separate fragments and this calls for caution; surgery is technically more difficult and, even with modern implants, stable fixation may be hindered because of poor bone quality. Pathological anatomy Intertrochanteric fractures are divided into stable and unstable varieties. The reverse oblique type of intertrochanteric fracture represents a subgroup of Type 4; it causes similar difficulties with fixation. Non-operative treatment may be appropriate for a small group who are too ill to undergo anaesthesia; traction in bed until there is sufficient reduction of pain to allow mobilization can yield reasonable results but much depends on the quality of nursing care and physical therapy (Kaplan, Miyamoto et al. Positioning the screw is important if it is to be prevented from cutting out of the osteoporotic bone. It should pass up the femoral neck to end within the centre of the femoral head, with the tip resting about 5 mm from the subchondral bone plate. The side plate should be long enough to accommodate at least 4 screws below the fracture line. In these cases a 95 degree screw-plate device or an intramedullary device with a hip screw gives more stable fixation. If closed reduction fails to achieve a satisfactory position, open reduction and manipulation of the fragments will be necessary. A large posteromedial fragment (often including the lesser trochanter) may need additional fixation. On the occasion that anatomical reduction proves impossible, a valgus osteotomy may be needed to allow the proximal fragment to abut securely against the femoral shaft (Dimon and Hughston 1967) (Figure 29. Postoperatively, exercises are started on the day after operation and the patient allowed up and partial weightbearing as soon as possible. If union is delayed, the implant 29 Injuries of the hip and femur (a) (b) (c) (d) (e) (f) 29. Types 1 and 2 fractures (a,b) can usually be held in good position with a compression screw and plate. If this is not possible, an osteotomy of the lateral cortex (c,d) will allow a screw to be inserted up to the femoral neck and into the head of the femur; this can be used as a lever to reduce the fracture so that the medial spike of the proximal fragment engages securely into the femoral canal; fixation is completed with a side plate. Reverse oblique fractures (e,f) are inherently unstable even after perfect reduction; here one can use an intramedullary device with an oblique screw that engages the femoral head. If healing is delayed (say beyond 6 months) the fracture probably will not join and further operation is advisable; the fragments are repositioned as anatomically as is feasible, the fixation device is applied more securely and bone grafts are packed around the fracture (Figure 29. Pathological fractures Intertrochanteric fractures may be due to metastatic disease or myeloma. Unless patients are terminally ill, fracture fixation is essential in order to ensure an acceptable quality of life for their remaining years. In addition to internal fixation, methylmethacrylate cement may be packed in the defect to improve stability. If there is involvement of the femoral neck, replacement with a cemented prosthesis may be preferable. The fracture is usually due to high velocity trauma; for example, falling from a height or a car accident. There is a high risk of complications, such as avascular necrosis, premature physeal closure and coxa vara. At birth the proximal end of the femur is entirely cartilaginous and for several years, as ossification proceeds, the area between the capital epiphysis and greater trochanter is unusually vulnerable to trauma. Moreover, between the ages of 4 and 8 the ligamentum teres contributes very little to the blood supply of the epiphysis; hence its susceptibility to post-traumatic ischaemia.
These infants should be followed up carefully, and additional iron supplementation may be required. However, many studies have shown that erythropoietin treatment is of limited benefit in reducing the number of transfusions once strict transfusion criteria are instituted. Complementary strategies to reduce phlebotomy losses and the use of conservative standardized transfusion criteria have contributed to significant reductions in transfusions. Association of Necrotizing Enterocolitis with anemia and packed red blood transfusions in preterm infants. A randomized trial to develop criteria for administering erythrocyte transfusions to anemic preterm infants 1 to 3 months of age. Role of leukocyte depletion in the prevention of transfusion-induced cytomegalovirus infection. American Academy of Pediatrics Committee on Nutrition: Iron-fortified infant formulas. Feeding iron-fortified premature formula during initial hospitalization to infants less than 1800 grams birth weight. Recombinant human erythropoietin stimulates erythropoiesis and reduces erythrocyte transfusions in very low birth weight preterm infants. The effect of epoetin beta (recombinant human erythropoietin) on the need for transfusion in very low birth weight infants. In which neonates does early recombinant human erythropoietin treatment prevent anemia of prematurity Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants. When the hematocrit increases to 60%, there is decreased oxygen delivery (1) (see Figure 46. As viscosity increases, there is impairment of tissue oxygenation and decreased glucose in plasma, leading to increased risk of microthrombus formation. If these events occur in the cerebral cortex, kidneys, or adrenal glands, significant damage may result. Hematocrit measurements vary greatly with site of sample, and capillary hematocrit may be up to 20% higher than venous (2). The mean venous hematocrit of term infants is 53% in cord blood, 60% at 2 hours of age, 57% at 6 hours of age, and 52% at 12 to 18 hours of age (2). Hyperviscosity is defined as viscosity 2 standard deviations greater than the mean (3). Blood viscosity, as described by Poiseuille, is the ratio of shear stress to shear rate and is dependent on such factors as the pressure gradient along the vessel, radius, length, and flow (4). The relationship between hematocrit and viscosity is nearly linear below a hematocrit of 60%, but viscosity increases exponentially at a hematocrit of 70% or greater (Figure 46. Other factors affect blood viscosity, including plasma proteins such as fibrinogen, local blood flow, and pH (3,4). The hyperviscosity syndrome is usually seen only in infants with venous hematocrits above 60%. When the cord is clamped within 1 minute after birth, the blood volume of the infant is approximately 80 mL/kg. When the cord is clamped 2 minutes after delivery, the blood volume of the infant is 90 mL/kg. In newborns with polycythemia, blood volume per kilogram of body weight varies inversely in relation to birth weight (see Figure 46. Maternal-to-fetal transfusion is diagnosed with the Kleihauer-Betke stain technique of acid elution to detect maternal cells in the circulation of the newborn (see Chap. Placental insufficiency (increased fetal erythropoiesis secondary to chronic intrauterine hypoxia) 1. Infants with congenital adrenal hyperplasia, Beckwith-Wiedemann syndrome, neonatal thyrotoxicosis, congenital hypothyroidism, trisomy 21, trisomy 13, trisomy 18. Clinical symptoms, syndromes, and laboratory abnormalities that have been described in association with polycythemia include the following: A. Poor feeding, lethargy, hypotonia, apnea, tremors, jitteriness, seizures, cerebral venous thrombosis. Cyanosis, tachypnea, heart murmur, congestive heart failure, cardiomegaly, elevated pulmonary vascular resistance, prominent vascular markings on chest x-ray. Decreased glomerular filtration, decreased sodium excretion, renal vein thrombosis, hematuria, proteinuria.

It is found where support matters most: the outer walls of all bones but especially the shafts of tubular bones, and the subchondral plates supporting articular cartilage. Between the lamellae lie osteocytes, bedded in lacunae which appear to be discrete but which are in fact connected by a network of fine canaliculi. The haversian canal offers a free surface lined by bone cells; its size varies, depending on whether the osteon is in a phase of resorption or formation. During resorption osteoclasts eat into the surrounding lamellae and the canal widens out; during formation osteoblasts lay down new lamellae on the inner surface and the canal closes down again. It shows the basic elements of compact bone: densely packed osteons, each made up of concentric layers of bone and osteocytes around a central haversian canal which contains the blood vessels; outer laminae of sub-periosteal bone; and similar laminae on the interior surface (endosteum) merging into a lattice of cancellous bone. At birth the cartilage model is complete and ossification has already begun at the centre of the diaphysis. After secondary ossification of the epiphyseal ends has begun, further growth in length takes place in the still cartilaginous zone between the extending area of diaphyseal bone and the epiphysis. In this way the still-cartilaginous zone between the ossifying diaphysis and the epiphysis gradually narrows down but does not disappear until late adolescence. This actively growing cartilage disc is called the physis, seated as it is between the epiphysis and the diaphysis. Coextensive with the epiphysis is a zone of resting chondrocytes in haphazard array. This merges into a proliferative zone in which the chondrocytes are lined up longitudinally; being capable of interstitial growth, they add progressively to the overall length of the bone. Close to the interface between cartilage and bone the cartilage becomes calcified (probably with the involvement of alkaline phosphatase produced by the hypertrophic cells); this zone of calcified cartilage finally undergoes osteoclastic resorption and, with the ingrowth of new blood vessels from the metaphysis, ossification. Woven bone is laid down on the calcified scaffolding and this in turn is replaced by lamellar bone which forms the newest part of the bone shaft, now called the metaphysis. It should be noted that a similar process takes place in the late stage of fracture repair. New bone is added to the outside by direct ossification at the deepest layer of the 121 7 7. Atlas of Orthopaedic Pathology: With Clinical and Radiological Correlations (2nd edition). During resorption each osteoclast forms a sealed attachment to the bone surface where the cell membrane folds into a characteristic ruffled border within which hydrochloric acid and proteolytic enzymes are secreted. At this low pH minerals in the matrix are dissolved and the organic components are destroyed by lysosomal enzymes. Calcium and phosphate ions are absorbed into the osteoclast vesicles from where they pass into the extracellular fluid and, ultimately, the blood stream. In cancellous bone this process results in thinning (and sometimes actual perforation) of existing trabeculae. During hyperactive bone resorption these processes are reflected in the appearance of hydroxyproline in the urine and a rise in serum calcium and phosphate levels. How else can a long bone retain its basic shape as the flared ends are constantly re-formed further and further from the midshaft during growth The internal architecture of the bone is also subject to remodelling, not only during growth but throughout life. Intramembranous periosteal new bone formation also occurs as a response to periosteal stripping due to trauma, infection or tumour growth, and its appearance is a useful radiographic pointer. Although it has Epiphyseal artery 7 Reserve cells Proliferative cells Metabolic and endocrine disorders Hypertrophic cells Degenerate cells Calcified zone Vascular invasion Ossification 7. Prompted by the osteoblasts, osteoclasts gather on a free bone surface and proceed to excavate a cavity.
Arthrography An arthrogram at this stage will clarify the anatomy of the hip and show whether there is an inturned limbus or any marked degree of acetabular dysplasia. Unilateral dislocation in the child over 8 years often leaves the child with a mobile hip and little pain. This is the justification for non-intervention, though in that case the child must accept the fact that gait is distinctly abnormal. If reduction is attempted it will require an open operation and acetabular reconstruc19. Therefore, in these cases, most surgeons avoid operation above the age of 6 years unless the hip is painful or deformity unusually severe. Complications Failed reduction Multiple attempts at treatment, with failure to achieve concentric reduction, may be worse than no treatment. The acetabulum remains undeveloped, the femoral head may be deformed, the neck is usually anteverted and the capsule is thickened and adherent. It is important to enquire also why reduction failed: is the dislocation part of a generalized condition, or a neuromuscular disorder associated with muscle imbalance The principles of treatment for children over 8 years are the same as those discussed above. Prevention is the best cure: forced manipulative reduction should not be allowed; traction should be gentle and in the neutral position; positions of extreme abduction must be avoided; soft-tissue release (adductor tenotomy) should precede closed reduction; and if difficulty is anticipated open reduction is preferable. Once the condition is established, there is no effective treatment except to avoid manipulation and weightbearing until the epiphysis has healed. In the mildest cases there will be no residual deformity, or at worst a femoral neck deformity which can be corrected by osteotomy. In severe cases the outcome may be flattening and mushrooming of the femoral head, shortening of the neck (with or without coxa vara), acetabular dysplasia and incongruency of the hip. Surgical correction of the proximal femur and pelvic osteotomy to reposition or deepen the acetabulum may be needed. Avascular necrosis A much-feared complication of treatment is ischaemia of the immature femoral head. It may occur at any age and any stage of treatment and is probably due to vascular injury or obstruction resulting from forceful reduction and hip splintage in abduction. The effects vary considerably: in the mildest cases the changes are confined to the ossific nucleus, which appears to be slightly distorted and irregular on x-ray. In more Persistent dislocation in adults Adults who appear to have managed quite well for many years may present in their thirties or forties with increasing discomfort due to an unreduced congenital dislocation. With bilateral dislocation, the loss of abduction may hamper sexual intercourse in women. The femoral head is seated above the acetabulum, which is shallow or completely obliterated. A new socket should be fashioned at the normal anatomical site; however, the pelvic wall is usually thin and it may be necessary to build up the roof of the socket with bone grafts. It is then difficult to bring the femoral head down to the level of the socket without risking damage to the sciatic nerve; if necessary, an osteotomy should be performed and a small segment of femoral bone removed to allow a safe fit. The proximal femur is usually very narrow and the neck may be markedly anteverted; this also may need correction when the osteotomy is performed, and special implants are available to fit the small medullary canal. The socket is unusually shallow, the roof is sloping and there is deficient coverage of the femoral head superolaterally and anteriorly; in some cases the hip subluxates. Clinical features During infancy, dysplasia may be clinically silent and only apparent on ultrasound examination. In children the condition is usually asymptomatic and discovered only when the pelvis is x-rayed for some other reason. The socket is shallow and the roof sloping, leaving much of the femoral head uncovered. Older adolescents and young adults may complain of pain over the lateral side of the hip, probably due to muscle fatigue and/or segmental overload towards the edge of the acetabulum. Some experience episodes of sharp pain in the groin, possibly the result of a labral tear or detachment.
All movements limited After severe injury, movement may be limited as a result of oedema and bruising. In osteoarthritis the capsule fibroses and movements become increasingly restricted, but pain occurs only at the extremes of motion. Although x-ray examination is essential, the clinical features can be highly informative. Size A large lump attached to bone, or a lump that is getting bigger, is nearly always a tumour. Site A lump near a joint is most likely to be a tumour (benign or malignant); a lump in the shaft may be fracture callus, inflammatory new bone or a tumour. Margin A benign tumour has a well-defined margin; malignant tumours, inflammatory lumps and callus have a vague edge. Consistency A benign tumour feels bony hard; malig- nant tumours often give the impression that they can be indented. Tenderness Lumps due to active inflammation, recent callus or a rapidly growing sarcoma are tender. Thus a torn and displaced meniscus may prevent extension of the knee but not flexion. Bone deformity may alter the arc of movement, such that it is limited in one direction (loss of abduction in coxa vara is an example) but movement in the opposite direction is full or even increased. Notwithstanding the extraordinary technical advances of the last few decades, it remains the most useful method of diagnostic imaging. The clinical diagnosis of cartilage-capped exostosis (osteochondroma) is confirmed by the x-rays. The radiographic image X-rays are produced by firing electrons at high speed onto a rotating anode. The more dense and impenetrable the tissue, the greater the x-ray attenuation and therefore the more blank, or white, the image that is captured. Similarly, the bright image of a metallic foreign body superimposed upon that of, say, the femoral condyles could mean that the foreign body is in front of, inside or behind the bone. Bulging outlines around a hip, for example, may suggest a joint effusion; and soft-tissue swelling around interphalangeal joints may be the first radiographic sign of rheumatoid arthritis. Tumours tend to displace fascial planes, whereas infection tends to obliterate them. Generalized change Localized change Is there a mass, soft tissue calcifica- tion, ossification, gas (from penetrating wound or gas-forming organism) or the presence of a radioopaque foreign body The process of interpreting this image should be as methodical as clinical examination. It is seductively easy to be led astray by some flagrant anomaly; systematic study is the only safeguard. For the pelvis, see if the shape is symmetrical with the bones in their normal positions, then look at the sacrum, the two innominate bones, the pubic rami and the ischial tuberosities, then the femoral heads and the upper ends of the femora, always comparing the two sides. Generalized change Take note of changes in bone `den- lesions think of metastases (including myeloma and lymphoma) and also multifocal infection. Localized change Focal abnormalities should be approached in the same way as one would conduct a clinical analysis of a soft tissue abnormality. Remember that benign lesions are usually well defined with sclerotic margins. Are there features suggestive of diffuse metastatic infiltration, either sclerotic or lytic It looks much wider in children than in adults because much of the epiphysis is still cartilaginous and therefore radiolucent. Loose bodies, if they are radio-opaque, appear as rounded patches overlying the normal structures. Further stages of joint destruction are revealed by irregularity of the radiographically visible bone ends and radiolucent cysts in the subchondral bone. Bony excrescences at the joint margins (osteophytes) are typical of osteoarthritis. In rheumatoid arthritis and psoriasis the erosions are peri-articular (at the bare area where the hyaline cartilage covering the joint has ended and the intracapsular bone is exposed to joint fluid).
References: